Alcoholic Liver Disease (ALD), also known as Alcohol-Related Liver Disease (ARLD), is a medical condition that often encompasses various liver-related conditions, primarily associated with the overconsumption of alcohol.
The various stages in Alcohol Liver Disease are Alcoholic Hepatitis, Alcoholic Fatty Liver Disease, and Chronic Hepatitis with Liver Cirrhosis. The liver is an incredible yet complex organ in the human body, which is responsible for regulating over 500 functions.
It not only detoxifies several metabolites, but also stores energy, stimulates hormones and proteins, regulates the storage of glycogen, blood sugars, and cholesterol, to name a few.
Located in the right upper quadrant of the abdomen, which approximately weighs around 1.5 kg with a width of 6 inches, it is both the heaviest organ and a gland. Often termed as an ‘accessory digestive organ’, it produces bile, which plays a crucial role in breaking down fat, aiding the process of digestion through emulsification.
Owing to its multidimensional functions, Liver is a vital organ in the human body, and its functions can be affected by various factors including viral infections causing Hepatitis A, Hepatitis B, Hepatitis C, D and E and many more conditions, but let’s discuss about the negative effects of alcohol on the liver.
The toxic effects of alcohol on the liver need no introduction. It is also a major health and economic problem, affecting millions of lives and families worldwide. Consuming alcohol up to 60 – 80 ml per day for around 2 decades would increase the risk of developing various ARLD conditions by 47%, and women are more prone to developing ARLD than men.
It is because 80% of the alcohol passes through the liver to get detoxified, and it aggravates inflammation by stimulating the production of cytokines, causing oxidative stress, acetaldehyde toxicity, lipid peroxidation, and leading to further swelling of the liver. Easy availability and affordability, the components in alcoholic beverages that could lead to addiction, are a few deterring factors for millions of liquor consumers to give up the habit. As a result, it is causing constant and permanent damage to this vital organ.
Alcoholic liver disease has three stages, and it can overlap between each stage.
- Alcoholic Fatty Liver Disease
- Alcoholic Hepatitis
- Liver Cirrhosis
Symptoms
ALD may not cause symptoms at first. They often show up only after the liver is badly affected, and can get worse after drinking heavily.
Early symptoms may include:
- Loss of energy and persistent fatigue
- Poor appetite and unintended weight loss
- Nausea or discomfort in the upper abdomen
- Visible red, spider-like blood vessels on the skin (spider angiomas)
As the disease progresses, symptoms may become more serious:
- Swelling in the legs (edema) or abdomen (ascites)
- Yellowing of the skin and eyes (jaundice)
- Redness on the palms of the hands
- Easy bruising and bleeding
- Mental confusion, forgetfulness, or difficulty concentrating (hepatic encephalopathy)
- Light-colored or pale stools
- Bleeding in the digestive tract
- In men: decreased libido, shrinking of the testicles, and breast enlargement (gynecomastia)
Risk factors
Several variables can increase the risk of developing alcoholic liver disease (ALD):
- Type of Alcohol Consumed: People who drink beer and liquor may have a higher risk of liver disease compared to those who consume wine.
- Gender: Females have a higher risk of developing alcoholic liver disease than males, even at the same levels of intake. Women are more likely to develop liver fibrosis, inflammation, and injury faster.
- Amount and Duration of Drinking: Consuming alcohol over several years increases the risk of ALD more in females than in males.
- Body Weight: Obesity or extra body weight increases the risk of developing liver disease in both men and women. This risk is higher with frequent alcohol usage.
- Viral Hepatitis: Having hepatitis C or other types of viral hepatitis, combined with regular alcohol consumption, raises the risk of liver damage.
- Genetic Factors: Variations in alcohol metabolism genes, such as ADH and ALDH, can increase the risk of developing alcoholic liver disease.
Complications
Common Complications of Alcoholic Liver Disease (ALD) include:
- Bleeding disorders (Coagulopathy)
- Fluid buildup in the abdominal area (ascites) carries a risk of becoming infected. (Spontaneous bacterial peritonitis)
- Swollen veins in the esophagus or stomach that can bleed easily and may be life-threatening(Esophageal varices)
- Increased blood pressure in the liver’s vessels due to impaired blood flow(Portal hypertension).
- A type of kidney failure that occurs in people with advanced liver disease(Hepatorenal syndrome).
- A form of liver cancer is more likely to develop in those with long-standing liver damage(Hepatocellular carcinoma).
Alcoholic Hepatitis
The next stage in Alcohol Liver Disease is Alcoholic Hepatitis, in which abnormal amounts of fat are deposited in the liver cells, causing an inflammatory response. It is often seen in binge boozers, as the liver undergoes enormous amounts of stress while filtering highly toxic substances.
The major reason behind this condition is in those who overconsume liquor in a short period of time, like a few months or a year, and the liver can fail due to acute illness. It can also happen in those who may not be regular drinkers, and other factors like obesity, genetics, sex, and ethnicity could be the triggers.
The adverse effects of Alcoholic Hepatitis are quite severe, as it can lead to enlarged veins that obstruct the flow of blood, causing heavy bleeding in the upper abdominal region and mimicking flu-like symptoms.
The patient may also suffer from ascites or fluid buildup in the stomach, confusion, slurred speech, kidney failure, and finally cirrhosis or scarring of the liver.
The worsening of Alcoholic Hepatitis can be prevented by completely staying away from liquor and other alcoholic substances. The patients are strictly required to take all medications and keep up with the doctor’s appointments.
Liver Cirrhosis
Liver Cirrhosis is the final stage in Alcohol alcohol-related liver Disease. At this stage, the healthy liver tissue gets replaced by scar tissue, which interferes with its functioning. It is often a result of cycles of liver damage caused by excessive consumption of alcohol, and in other words, a healthy liver is scarred for life.
As the condition worsens, more and more scar tissues replace the liver, causing severe swelling in the legs and abdominal regions, and it is often a result of massive fluid buildup. Splenomegaly or enlargement of the spleen, internal bleeding, and portal hypertension or high blood pressure in the veins that facilitate blood supply to the liver from the spleen and intestines are other complications.
Portal Hypertension
Portal Hypertension is a condition in which the blood pressure builds up in the intestinal veins, collectively known as the Portal Venous System. Cirrhosis can cause severe damage to the liver, blocking blood flow from the intestines, causing increased pressure in the Portal Venous System.
As pressure builds up, blood finds other ways of bypassing the obstructed liver, causing these veins to become turgid and rupture. An internal rupture in the intestine leads to blood vomiting or blood in the stools, and it is a life-threatening emergency.
The patient suffering from this condition should be immediately wheeled into the hospital. The expert doctor can perform a minimally invasive procedure called endoscopy to arrest the bleeding.
The further course of treatment would depend upon taking stock of the complete situation after running other diagnostic tests.
Exams and Tests
During your physical exam, your doctor might look for:
- An enlarged liver or spleen.
- Red hands with spider-like blood vessels on the skin.
- Jaundice is a condition that results in a yellow tint to the skin and eyes.
- Swollen abdomen owing to fluid accumulation.
- Gynecomastia (excess breast tissue) and smaller testicles in men.
- Widened veins on the abdominal wall.
Recommended testing may include:
Blood tests like these:
- Complete blood count (CBC).
- Liver Function Tests
- Coagulation studies.
Imaging tests:
- Abdominal ultrasound
- CT scan of the abdomen
- Ultrasound elastography to assess liver stiffness
- Liver biopsy (in some cases)
- Further testing may be needed to identify or exclude other potential causes of liver disease.
Treatment
The first line of treatment in Alcohol Related Liver Disease is staying away from alcoholic substances completely. Abstaining from alcohol can reverse the early stages of this condition within 2 weeks as the Liver clears out all deposited fat.
It is quite crucial not to resume the habit of drinking, as the symptoms can recur soon after alcohol enters the body. However, in the case of addicts, the withdrawal should be done with the guidance of an expert doctor, as sudden stoppage could lead to withdrawal syndrome, which could be life-threatening. In cases of extreme alcohol addiction, the expert may also recommend counselling and Cognitive Behavioral Therapy to come out of the habit completely.
Besides abstaining from alcohol, the patient should also take all the prescribed medications on time and keep up with the regular appointments with the doctors.
Lifestyle changes are equally important in dealing with this condition. The overweight patients would be advised to lose weight, eat healthy, and quit smoking for faster recovery.
However, if any of the above conditions worsen, the treatment depends on what stage the patient is in. Unless the last stage of cirrhosis has set in, stopping alcohol is key.
If cirrhosis is already present, it becomes vital to completely stop alcohol consumption and undergo thorough diagnostic evaluations such as blood tests and an abdominal CT scan to check for malignancy, which is a common complication in a cirrhotic liver.
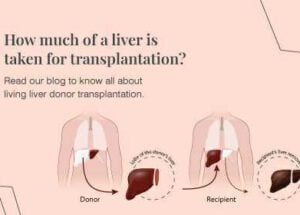
If the patient is diagnosed with any of the complications, and it is suggested that there is little or no hope of reversing the damage to the Liver, transplantation of the liver is to be considered as a life-saving measure
The criteria for offering liver transplantation to these patients are multifactorial and involve continued abstinence as a key. Also, it is crucial to identify which patients will benefit from transplantation, as liver transplantation in itself is a major undertaking and requires a lifelong commitment from the patient to remain abstinent and to adhere to immunosuppression medication.
Prevention
Lifestyle changes, which include;
- Keep your weight in check.
- Have a well-rounded diet.
- Engage in regular exercise.
- Limit alcohol or stop alcohol consumption.
- Take medications as directed.
- Get Screened Frequently
- Regular liver exams could aid in the early detection of issues, particularly if you have recognized risk factors like obesity or drinking.
- Take care of medical issues.
- Control conditions like hepatitis and diabetes to prevent liver damage.
- Ask for assistance when required.
- Having trouble cutting back on alcohol or your lifestyle? Medical advice and support groups can have a big influence.
When to Consult a Doctor
Consult your doctor if you:
- Notice the symptoms of alcoholic liver damage.
- Experience health problems after a long period of frequent drinking.
- Are you afraid that drinking may impair your liver?
Seek urgent medical assistance if you have:
- New or worsening discomfort in the abdomen or chest
- Sudden abdominal swelling (ascites).
- Fever above 101°F (38.3°C).
Rela Institute of Liver Disease & Transplantation, equipped with advanced liver care facilities and highly skilled liver specialists for the treatment of alcoholic liver diseases, offers a comprehensive disease management program to prevent liver damage due to alcohol consumption. In cases of severe alcohol abuse, the liver is likely to develop a fatal stage called cirrhosis. As liver cirrhosis leads to a high risk of mortality due to scarring of the liver, liver transplant is opted for as treatment for patients to improve their life expectancy. Rela Hospital, with 1400 liver transplants in Tamil Nadu to its credit, is acknowledged as one of the best liver transplant centres in India. The best liver transplant surgeons in Chennai with world-class expertise in liver transplantation offer a coordinated multidisciplinary liver transplant program at Rela Hospital, making it the best multispeciality hospital for liver transplantation in Chennai, India.