Importance of MELD Score in Liver Transplantation
August 13, 2019

What Does MELD Score Mean?
A very accurate scoring system has been developed for predicting survival in adult patients with liver disease. This system is termed the Model for End-Stage Liver Disease, or MELD. Earlier, patients on the liver transplant waiting list were prioritized to receive a liver transplant according to their “status.” Status depended upon blood tests, signs of severe liver disease and the amount of time spent on the list.
What is a MELD Score?
The MELD score was developed by the United Network for Organ Sharing (UNOS), a non-profit charitable organization, which operates the Organ Procurement and Transplantation Network (OPTN). On an ongoing basis, the OPTN/UNOS evaluates new advances and research and adapts these into new policies to best serve patients waiting for transplants. As part of this process, the OPTN/UNOS developed this system for prioritizing candidates waiting for liver transplants based on statistical formulas that are very accurate for predicting who needs a liver transplant most urgently.
Understanding the MELD Score System
Under the MELD scoring system, each patient is given a MELD score based on three lab tests:
- Bilirubin, which measures how effectively the liver makes bile
- INR prothrombin time, which measures the liver’s ability to make clotting factors
- Creatinine, which measures kidney function, often tied closely to liver function
This system assures that donated livers go to the patients in greatest need at that moment. Depending on how critical the disease is, MELD score may be recalculated as often as once a week.
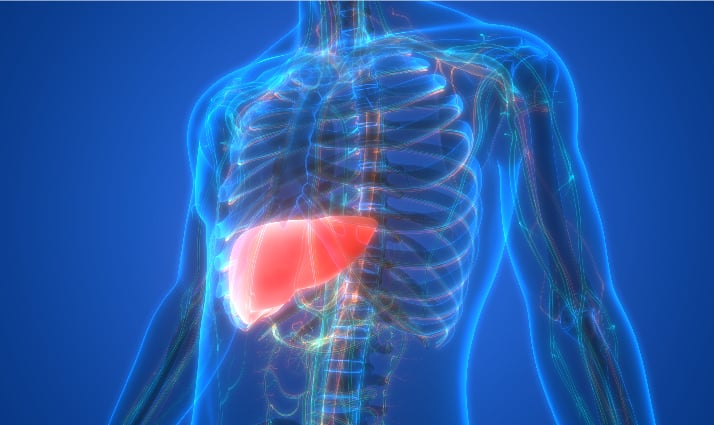
Why is the MELD score important in liver transplantation?
The MELD score plays a crucial role in liver transplantation because it helps prioritise patients based on the severity of their liver disease and their need for a transplant. By considering factors such as bilirubin, INR prothrombin time and creatinine levels, the MELD score provides a standardised method for assessing the urgency of transplantation.
This ensures that livers are allocated to those who need them most urgently, improving the chances of successful outcomes for recipients. Additionally, the MELD score helps optimise the use of available donor organs, maximising the benefit to patients awaiting transplantation. Overall, the MELD score serves as a vital tool in the fair and efficient allocation of liver transplants, ultimately saving lives and improving patient outcomes.
How is the MELD Score Calculated?
Typical MELD scores are recalculated, if these are:
- 25 or higher: Every week
- 19-24: Every 30 days
- 11-18: Every three months
- 10 or less: Once a year
Factors Influencing Liver Transplant Allocation
However, MELD score isn’t the only factor. Other considerations include:
- blood type
- body size relative to the donor’s
- Geographical considerations (i.e. how close patient is to the donor liver)
- Current supply of, and demand for, deceased donor livers
In case of patients with a MELD score less than 15, they are often not listed for a liver transplant because their chance of receiving a liver through traditional allocation is so low, a living-donor liver transplant offers a life-saving option and the opportunity to receive a transplant sooner. By exploring a living donor transplant, patients with a low MELD score can still be considered for a liver transplant.
Living Donor Transplantation for Low MELD Scores
-
Exploring alternatives for patients with low MELD scores:
Patients with low MELD scores, typically below 15, often face prolonged waiting times for a deceased donor liver due to their lower transplant urgency. Living donor transplantation emerges as a promising solution for these individuals, offering them an opportunity to receive a liver transplant sooner rather than later.
-
Benefits and considerations of living donor transplants:
- Timely Treatment: Living donor transplants provide patients with lower MELD scores the chance to undergo transplantation sooner. This can potentially prevent the progression of their liver disease and improve their overall health outcomes.
- Reduced Wait Times: Living donor transplants bypass waitlists, cutting patient wait times, reducing disease risks. They offer timely access to livers, lowering chances of health complications.
- Improved Outcomes: Studies suggest living donor liver transplants offer superior outcomes. Donor organs are healthier, less wait time reduces health risks.
- Donor Compatibility: Living donor transplantation allows for better matching between donor and recipient, potentially reducing the risk of organ rejection. Hence, it improving overall transplant success rates.
- Emotional Benefits: Living donor transplantation is emotionally rewarding. It’s a direct way to help a loved one in need.
Considerations:
- Surgical Risks: Living donor transplantation is major surgery. It carries risks like bleeding, infection, and anaesthesia complications.
- Donor Consent: Ensure living donor fully understands risks. Consent must be voluntary, without coercion.
- Long-term Impact on Donor Health: While living donors can lead normal lives with one healthy liver lobe, there may be long-term implications for their health, including a slightly increased risk of developing liver-related complications later in life.
- Psychological Impact: Recipients and donors face emotional stress. Surgery, recovery and complications cause anxiety.
-
Expanding options for those with lower transplant urgency:
Living donor transplantation offers a valuable option for patients with lower transplant urgency. Allowing them to access transplantation sooner and potentially improving their quality of life and long-term outcomes. By expanding the range of available treatment options, living donor transplantation plays a crucial role in addressing the needs of all patients awaiting liver transplantation, regardless of their MELD score.
Conclusion
The MELD score serves as a vital tool in prioritizing patients for liver transplantation, ensuring that those in most urgent need receive timely treatment. While the score is a significant factor, various considerations, such as blood type and geographical location, also influence organ allocation. For patients with low MELD scores, living donor transplantation emerges as a promising alternative, offering timely access to transplantation and potentially improving overall health outcomes.
However, it’s essential to recognize the risks and considerations associated with living donor transplantation, including surgical risks and long-term impacts on donor health. Ultimately, living donor transplantation expands treatment options, providing hope and improving the quality of life for patients with lower transplant urgency.
WHY Rela Hospital?
MELD scores are accurately calculated in Rela Hospital, the best hospital for liver transplantation in India. As we have the best liver transplant specialists in India, you can be assured that if your MELD scores are higher, we will make every effort to ensure that you are our priority. As part of our liver transplant program in India, we ensure that our patients get the priority they deserve depending on the severity of their disease.
Frequently Asked Questions
1. What is the significance of the MELD score?
The MELD score is crucial in liver transplants. It helps doctors prioritize who needs a new liver the most urgently. Patients with higher scores, indicating more severe liver disease, have a better chance of receiving a transplant sooner, ensuring fair allocation of limited donor organs.
2. What MELD score is needed for transplant?
The MELD score needed for a transplant varies but generally, higher scores indicate greater urgency. Patients with MELD scores typically above 15 are considered for transplant, with higher scores prioritized.
3. Are there any limitations or criticisms of the MELD score system?
Yes, there are limitations to the MELD score system. It may not fully account for individual patient factors, such as overall health or complications. Additionally, some argue it doesn’t consider the severity of symptoms or quality of life.