What is a liver transplant?
A liver transplant is a complex surgical procedure in which a diseased or malfunctioning liver is replaced with a healthy liver from a deceased or living donor. The liver is a vital organ responsible for various essential functions, including detoxification, metabolism of nutrients, production of bile, and synthesis of proteins. When the liver becomes severely damaged or fails to function properly, a liver transplant may be the only viable option to sustain life.
Why would someone need to have a liver transplant?
Liver transplant becomes necessary when an individual’s liver is unable to perform its functions adequately due to liver failure, which can occur in both acute and chronic forms.
- Acute liver failure: This occurs suddenly and is often caused by conditions such as drug overdose, viral hepatitis, autoimmune hepatitis, or acute fatty liver of pregnancy. Acute liver failure can rapidly lead to life-threatening complications and requires immediate medical intervention.
- Chronic liver failure: This develops gradually over time and is commonly associated with chronic liver diseases like cirrhosis, hepatitis B or C infection, non-alcoholic fatty liver disease (NAFLD), or alcoholic liver disease. In chronic liver failure, the liver progressively loses its ability to function properly, leading to complications that can be fatal if left untreated.
Liver transplantation may also be performed for individuals with primary liver cancer, specifically hepatocellular carcinoma (HCC), which is the most common form of liver cancer.
How long can you live without a liver transplant?
The survival rate without a liver transplant depends on the severity of liver disease and the underlying cause. Acute liver failure is a medical emergency, and without a transplant or intervention, survival is usually measured in days to weeks. In cases of chronic liver failure, the prognosis is more variable. Some individuals may live for several years with medical management, while others may experience a rapid decline in health.
How common are liver transplants?
Liver transplantation has become a well-established procedure worldwide. The number of liver transplants performed each year varies by country and region, but it is estimated that thousands of liver transplants are performed globally. The demand for liver transplants often exceeds the supply of donor organs, leading to waiting lists and the need for strict criteria for patient selection.
Which Tests Are Required Before Getting a Liver Transplant?
Before undergoing a liver transplant, a comprehensive evaluation is performed to assess the patient’s suitability for the procedure. This evaluation typically includes a thorough medical history, physical examination, and a series of tests, such as blood tests, imaging studies (such as CT scan or MRI), liver biopsy, and cardiac evaluation. These tests help determine the severity of liver disease, identify potential complications, and assess the patient’s overall health.
How are donor livers matched with transplant recipients?
The matching of donor’s livers with transplant recipients is a complex process that involves several factors. The primary considerations for matching include blood type compatibility, body size compatibility, and the severity of the recipient’s condition. The United Network for Organ Sharing (UNOS) and similar organisations in different countries maintain extensive waiting lists and allocate organs based on a scoring system that considers these factors.
Where Does a Liver for a Transplant Come From?
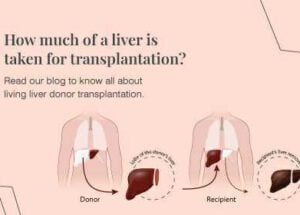
Donor livers for transplantation come from two main sources: deceased donors and living donors.
- Deceased donors: Deceased donor livers are obtained from individuals who have experienced brain death or cardiac death. These organs are carefully evaluated to ensure they are healthy and suitable for transplantation. Deceased donor livers are in limited supply, and the availability depends on the number of individuals who register as organ donors and the occurrence of suitable organ donations.
- Living donors: In some cases, a living person can donate a portion of their liver for transplantation. The liver has a remarkable ability to regenerate, allowing the remaining liver in both the donor and the recipient to grow and regain full function. Living donor liver transplantation offers the advantage of avoiding the waiting list and can be scheduled at a convenient time for both the donor and recipient.
Self-care after liver transplant
- Attending regular follow-up appointments: Regular visits to the transplant center are essential to monitor the function of the new liver, assess medication levels, and address any concerns or complications that may arise.
- Maintaining a healthy lifestyle: Adopting a healthy lifestyle is crucial for long-term health after a liver transplant. This includes:
- Following a balanced diet: A dietitian can provide personalized guidance on maintaining a nutritious diet that supports liver health and prevents weight gain or malnutrition. It is important to limit sodium intake, consume adequate protein, and avoid foods that may interact with immunosuppressant medications.
- Engaging in regular physical activity: Physical activity helps maintain overall health, cardiovascular fitness, and weight management. However, it is important to consult with the transplant team before starting any exercise regimen to ensure it is safe and appropriate for individual circumstances.
- Avoiding alcohol and certain medications: Alcohol can have detrimental effects on the liver, and it is crucial to abstain from alcohol completely after a liver transplant. Certain medications, including over-the-counter drugs, herbal supplements, and high-dose painkillers, can be harmful to the liver and should be avoided or used with caution. It is important to consult with the transplant team or pharmacist before taking any new medications.
- Emotional well-being: A liver transplant can be a life-changing experience, and it is important to prioritize emotional well-being. This may involve seeking support from mental health professionals, joining support groups, or engaging in activities that promote relaxation and stress management.
- Support from healthcare professionals and loved ones: Building a strong support network is crucial during the recovery process. Regular communication and collaboration with the transplant team, including surgeons, nurses, dietitians, and pharmacists, can help address any concerns or questions that may arise. Family and friends can also provide emotional support and assistance with daily activities.
When and who to consult?
- It is important to consult the Liver Transplant Surgeon if any new symptoms or complications arise, such as fever, pain, jaundice, or changes in appetite or urine output.
- Regular follow-up appointments with the transplant team are necessary to monitor the function of the transplanted liver and adjust medications as needed. These appointments may include visits to transplant surgeons, hepatologists, and other specialists involved in post-transplant care.
- Consulting with a dietitian can provide personalised nutrition and dietary modification guidance to support liver health and overall well-being.
- Mental health professionals can offer support and guidance for emotional well-being before and after the transplant.
- Pharmacists can provide information on medication interactions and ensure that any new medications prescribed or over-the-counter drugs are safe for the transplanted liver.
- In case of an emergency, it is important to contact the transplant centre or the designated emergency contact provided by the transplant team.
Remember, self-care after a liver transplant is essential for maintaining the health of the transplanted liver and overall well-being. Regular communication and collaboration with healthcare professionals and a supportive network of loved ones can contribute to a successful recovery and long-term success after the transplant.
People also ask
1. Can a living person donate a liver?
Yes, living individuals can donate a portion of their liver for transplantation. The liver has the remarkable ability to regenerate, allowing both the remaining liver in the donor and the transplanted liver in the recipient to grow and regain full function. Living donor liver transplantation offers an alternative to deceased donor transplantation and can significantly reduce waiting times.
2. How serious is a liver transplant?
Liver transplant is a major surgical procedure that carries risks, like any other surgery. Potential complications include bleeding, infection, blood clots, organ rejection, and side effects from immunosuppressant medications. However, advancements in surgical techniques, perioperative care, and post-transplant management have significantly improved liver transplantation’s success rates and outcomes.
3. How is a liver transplant done?
The surgical procedure for liver transplantation involves removing the diseased liver and replacing it with a healthy liver from a deceased or living donor. The surgeon carefully connects the blood vessels and bile ducts of the new liver to those of the recipient. The surgery typically lasts several hours, and the patient is placed under general anesthesia to ensure comfort and safety. Following the surgery, the patient is closely monitored in the intensive care unit and gradually transitioned to a regular hospital room as they recover.