Budd Chiari Syndrome
A rare condition that affects just one in every million adults, Budd-Chiari syndrome results from blood clots that partially or completely block blood flow out of the liver. This blockage could occur anywhere from the small or large veins that transport blood from the hepatic veins to the inferior vena cava. It is also known as Hepatic Vein Thrombosis (HVT).
Causes
Budd Chiari Syndrome can be due to genetic reasons, diseases or medication. Whatever causes blood clotting in the liver’s veins causes HVT.
Its most common causes are:
- Congenital blood disorders
- Vein inflammation
- Liver cancer and trauma
- Autoimmune disorders
- Infections
- Pregnancy
- Inflammatory disorders
- Birth control pills
- Connective tissue disorders
- Immunosuppressant drugs
Symptoms
- Nausea
- Jaundice
- Fatigue
- Abdominal pain
- Fluid accumulation in the abdomen
- Enlarged spleen
- Severe bleeding in the oesophagus
- Narrow or blocked veins
Types
Budd-Chiari syndrome (BCS) can be classified in several ways, including by disease duration, location of obstruction, and whether it’s primary or secondary. Acute, subacute, and chronic are common classifications based on disease duration. Primary BCS results from hepatic vein blockage, while secondary BCS involves external compression or invasion.
Here’s a detailed breakdown:
1. By Duration/Onset:
- Acute BCS: Symptoms develop rapidly (over weeks) and can include severe abdominal pain, ascites, and liver failure.
- Subacute BCS: Symptoms develop more gradually (over months) and can include less severe ascites and portal hypertension.
- Chronic BCS: Symptoms develop slowly over a long period, potentially leading to cirrhosis and its complications.
2. By Location of Obstruction:
- Hepatic vein occlusion: Blockage of one or more hepatic veins.
- Inferior vena cava (IVC) occlusion: Blockage of the IVC, sometimes with involvement of the hepatic veins.
- Mixed type: Involves a combination of hepatic vein and IVC obstruction.
3. By Cause:
- Primary BCS: The obstruction originates from within the hepatic veins, often due to thrombosis or a membrane.
- Secondary BCS: The obstruction is caused by something outside the veins, such as tumours, cysts, or external compression.
4. Other Classifications:
- Fulminant BCS: A rare, severe form characterised by hepatic encephalopathy and rapid liver failure.
- Acute on chronic BCS: An acute exacerbation of chronic BCS, often triggered by a new event.
Diagnosis
Budd-Chiari syndrome (BCS) diagnosis is based on clinical findings, imaging, and sometimes liver biopsy.
Diagnostic Steps:
1. Clinical Suspicion:
Doctors suspect BCS in patients with symptoms like abdominal pain, ascites (fluid buildup in the abdomen), jaundice, and an enlarged liver, especially when these occur without a clear cause. Conditions that predispose to blood clots are also considered.
2. Initial Imaging: Doppler Ultrasound:
This test is usually the first step and can reveal abnormalities in the hepatic veins, like narrowed or blocked vessels, abnormal blood flow, and signs of portal hypertension.
3. Further Imaging: CT and MRI:
- CT scans: can show an enlarged liver, ascites, and signs of hepatic vein obstruction.
- MRI scans are valuable for assessing liver morphology, detecting subtle changes, and differentiating BCS from other liver conditions. MRI can also evaluate the extent of liver damage and identify complications.
4. Liver Biopsy:
If non-invasive imaging is inconclusive or if the thrombosis is limited to small intrahepatic veins, a liver biopsy may be necessary. The biopsy can reveal signs of blood outflow obstruction, such as congestion, necrosis, or fibrosis.
5. Laboratory Tests:
Blood tests are done to assess liver function and rule out other potential causes of liver disease. Tests for thrombophilia (tendency to clot) are also important.
6. Venography (If Needed):
In some cases, venography (X-ray of veins) may be used to visualise the hepatic veins and confirm the diagnosis, especially if other tests are inconclusive.
Treatment
Treatment for Budd-Chiari syndrome focuses on dissolving clots or widening narrowed hepatic veins or the IVC to reduce liver swelling and prevent scarring. Treatments will manage the underlying condition that caused you to develop clots. Issues like portal hypertension, characterised by elevated blood pressure in the portal vein, require careful management.
Medications
Doctors may prescribe anticoagulants, like heparin or warfarin, to help break down blood clots.
Nonsurgical Procedures
Your doctor might perform a procedure to reroute blood flow and reduce pressure in your vessels. These procedures include:
- Transjugular intrahepatic portosystemic shunt (TIPS): The doctor makes a tunnel through your liver with a needle. These procedures link the portal vein, which brings blood to the liver, with one of the hepatic veins, which carries blood away from the liver. Using X-ray guidance, a stent (a small metal tube) is inserted into the tunnel to keep it open.
- Percutaneous transluminal angioplasty: A catheter (a thin, hollow tube with a balloon at the tip) is inserted through your skin and into a blood vessel. They will guide the catheter to the clot or the narrowed area. When the catheter arrives at the targeted area, the doctor inflates a balloon to expand the vein. A stent can be inserted at the location to maintain the vein’s openness.
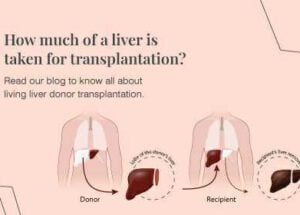
Liver Transplant
If treatments haven’t helped or aren’t an option, you may need a liver transplant. This is particularly necessary if you have liver failure, cirrhosis, or complications like variceal bleeding or ascites that don’t respond to medication.
Risk Factors
Several risk factors have been linked to Budd-Chiari Syndrome, which may raise the chances of developing the disorder. Some of them include:
- Oral contraceptives administration: The use of estrogen-containing oral contraceptives increases the risk of developing Budd-Chiari syndrome twofold. If you have thrombogenic diseases, oral contraceptives seem to increase the risk of thrombosis.
- Trauma: If there is severe trauma, the veins over the liver may burst, and this may result in a dramatic consequence of developing a syndrome (group of symptoms).
- Inflammatory diseases: Anyone with inflammatory disorders such as inflammatory bowel disease or Behcet’s disease is at a greater risk for developing thromboembolic complications, which may eventually lead to Budd-Chiari syndrome.
- Coronavirus disease (COVID-19): A study done in 2023 demonstrated that inflammatory and coagulation disorders associated with coronavirus disease 2019 (COVID-19) can cause Budd-Chiari syndrome.
- Cancers: Several cancers, such as hepatocellular carcinoma, may have the tendency to cause Budd-Chiari syndrome through invasion of venous outflow.
Complications
Budd-Chiari syndrome, characterised by the obstruction of hepatic venous outflow, can lead to several serious complications. These include portal hypertension, hepatic encephalopathy, variceal haemorrhage, hepatorenal syndrome, bacterial peritonitis, and hepatocellular carcinoma. Untreated, it can result in progressive liver failure and death.
Untreated Budd-Chiari syndrome generally may have complications such as:
- Hepatic encephalopathy (the loss of brain function resulting from the liver’s inability to eliminate toxins from the blood)
- Variceal haemorrhage (rupture of blood vessels located all over the digestive system)
- Hepatorenal syndrome (Kidney failure due to liver dysfunction)
- Portal hypertension (increased blood pressure in the vein that carries deoxygenated blood to the liver from the intestines)
- Bacterial peritonitis (infection of abdominal fluid) in the presence of ascites
- Hepatocellular carcinoma (liver cancer)
Prevention
To prevent this disorder, it is important to manage the risk factors that give rise to Budd-Chiari Syndrome. You could focus on:
- Thrombosis risk management: Taking care of diseases that raise the risk of thrombosis is essential since Budd-Chiari syndrome is frequently brought on by blood clots in the hepatic veins.
- Oral Contraceptives and Pregnancy: In women, particularly those of childbearing age, careful consideration of oral contraceptive use and monitoring during pregnancy is important due to the increased risk of blood clots.
- Surveillance throughout the pregnancy: Many women of childbearing age suffer from Budd-Chiari syndrome. If you have an underlying prothrombotic disease, pregnancy can exacerbate your condition and lead to Budd-Chiari syndrome. Additional prothrombotic disease screening must be conducted for these women.
- Drug use monitoring: Certain drugs may make clotting more likely. Use of them should only be done under medical supervision.
- Lifestyle modifications: Obesity caused by a lack of exercise is causing a rise in thrombotic illnesses such as venous thromboembolism. Since thrombotic diseases can cause blockages in blood vessels, it is highly recommended to maintain a healthy weight.
- Inflammatory Bowel Disease (IBD): IBD can increase the risk of blood clots, so managing IBD effectively can be a preventative measure.
Frequently Asked Questions
1. What is the life expectancy with Budd-Chiari?
If left untreated, a complete blockage of the hepatic vein can lead to liver failure, with most patients not surviving beyond three to five years. A liver transplant can help you live longer. Research indicates that people generally survive longer when their veins are partially obstructed rather than completely blocked. However, with prompt diagnosis and treatment, the 5-year survival rate can be as high as 90%. Factors like the extent of vein blockage and the presence of underlying conditions significantly influence long-term prognosis.
2. Is Budd-Chiari syndrome curable?
Budd-Chiari syndrome is potentially curable, especially when diagnosed and treated early. While it can be a chronic condition, effective treatments like anticoagulants, angioplasty, shunting, and in severe cases, liver transplantation, can significantly improve outcomes and even lead to a cure in some instances.
3. What genders are predominantly affected by Budd-Chiari syndrome?
Budd-Chiari syndrome affects both males and females, but the gender distribution varies by geographical location. In Western countries, it is more commonly diagnosed in females, while in Asian countries, it is more common in males.
4. What is the difference between portal vein thrombosis and Budd-Chiari syndrome?
Portal vein thrombosis (PVT) and Budd-Chiari syndrome (BCS) are both conditions involving blood clots in the liver’s veins, but they affect different vessels. PVT involves a clot in the portal vein, which carries blood from the digestive system to the liver, while BCS involves a clot in the hepatic veins, which carry blood away from the liver. This leads to different clinical presentations and management strategies.