What is Wilson’s Disease?
Wilson’s disease, also known as hepatolenticular degeneration, is a rare genetic disorder characterized by the accumulation of copper in various organs of the body, particularly the liver and brain. The liver normally releases excess copper into the bile, which is then eliminated through the digestive system. In individuals with Wilson’s disease, copper is not properly excreted, leading to its accumulation and subsequent damage to vital organs.
Who does Wilson’s Disease Affect?
Wilson’s disease can affect both males and females of all ethnic backgrounds. It usually manifests between the ages of 5 and 35, with the majority of cases diagnosed during adolescence or early adulthood. However, it can occur at any age, from infancy to late adulthood.
How Does Wilson’s Disease Affect the Body?
In Wilson’s disease, the liver’s ability to process and eliminate excess copper is impaired. The accumulated copper gradually builds up and gets released into the bloodstream, affecting various organs throughout the body, including the liver, brain, kidneys, and cornea. The excessive copper causes oxidative damage, leading to inflammation, scarring, and dysfunction of these organs.
Symptoms of Wilson’s Disease:
The symptoms of Wilson’s disease can vary widely, and the severity of the disease can range from mild to life-threatening. The most common symptoms include:
1. Hepatic Symptoms
- Fatigue and weakness
- Abdominal pain and swelling
- Jaundice (yellowing of the skin and eyes)
- Easy bruising and bleeding
- Fluid retention (edema)
2 .Neurological Symptoms
- Tremors or involuntary movements
- Difficulty speaking or swallowing
- Personality changes or mood swings
- Anxiety, depression, or psychosis
- Difficulty with coordination and balance
- Slurred speech
- Rigidity or stiffness
3. Ocular Symptoms
- Kayser-Fleischer rings: A brownish ring around the cornea caused by copper deposition.
- Eye abnormalities: Eye movement abnormalities, decreased vision, or light sensitivity.
Causes of Wilson’s Disease
Wilson’s disease is caused by mutations in the ATP7B gene, which is responsible for producing a protein that helps transport copper in the body. The defective ATP7B gene impairs the liver’s ability to release copper into the bile, resulting in its accumulation. Wilson’s disease is an autosomal recessive disorder, meaning an affected individual must inherit two copies of the mutated gene, one from each parent.
Inheritance of Wilson’s Disease
Wilson’s disease is inherited in an autosomal recessive manner. This means that an individual must inherit two copies of the mutated ATP7B gene, one from each parent, to develop the disease. If both parents carry one copy of the mutated gene, each of their children will have a 25% chance of inheriting two copies and developing Wilson’s disease.
Diagnosis of Wilson’s Disease: Diagnosing Wilson’s disease requires a combination of clinical evaluation, medical history assessment, and specialized laboratory tests. The following tests are commonly used for diagnosis:
1. Blood and Urine Tests
- Copper and ceruloplasmin levels: Elevated copper levels and decreased ceruloplasmin levels indicate Wilson’s disease.
- Liver function tests: Abnormal liver enzymes may be indicative of liver damage.
2. Genetic Testing
- DNA analysis to identify mutations in the ATP7B gene.
3. Imaging
- Abdominal ultrasound or MRI to assess liver and spleen abnormalities.
Treatment of Wilson’s Disease:
The treatment of Wilson’s disease aims to reduce copper levels in the body and prevent further copper accumulation. It typically involves two main approaches
1. Dietary Modifications
- Avoiding foods high in copper, such as organ meats, shellfish, nuts, and chocolate.
- Maintaining a low-copper diet to limit copper intake.
2. Copper-Chelating Medications
- Medications that bind to copper and enhance its elimination from the body.
- Prescribed based on the individual’s symptoms, age, and overall health.
Dietary Considerations: People with Wilson’s disease should follow a low-copper diet to minimize copper intake. They should avoid or limit the consumption of high-copper foods, such as organ meats, shellfish, mushrooms, chocolate, nuts, and legumes. It is advisable to consult a registered dietitian or healthcare professional for personalized dietary recommendations
Self-Care Practices
Individuals with Wilson’s disease can take certain steps to manage their condition and promote overall well-being. These include:
- Adhering to prescribed medications and dietary guidelines.
- Regularly monitoring copper levels and liver function.
- Engaging in regular physical activity, with the advice of healthcare professionals.
- Seeking support from support groups or counseling to cope with the emotional aspects of the disease.
When and Who to Consult?
If you experience symptoms such as unexplained fatigue, jaundice, tremors, or changes in behavior, it is crucial to consult a healthcare professional. Medical experts specializing in hepatology or genetics can provide a proper diagnosis, treatment, and ongoing management of Wilson’s disease.
What questions should I ask my doctor?
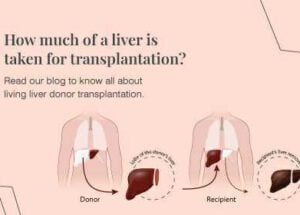
- Will I need a liver transplant?
- What are the side effects of the medicine you prescribed to treat Wilson disease?
- If I become pregnant, will my child have Wilson disease?
- Can I take my medicine if I get pregnant?
- How long should I take the medicine you prescribed?
People Also Ask
1. Can Wilson’s disease be cured?
While there is no known cure for Wilson’s disease, it can be effectively managed with lifelong treatment and adherence to dietary modifications.
2. Can Wilson’s disease be fatal?
If left untreated, Wilson’s disease can lead to severe liver damage, neurological complications, and even death. Early diagnosis and appropriate treatment significantly improve long-term outcomes.
3. Can Wilson’s disease skip a generation?
Wilson’s disease can appear to skip generations if individuals with a single copy of the mutated gene (carriers) do not show symptoms. However, carriers can pass on the disease to their children.
4. Can pregnancy worsen Wilson’s disease symptoms?
Pregnancy can potentially worsen Wilson’s disease symptoms due to hormonal changes and increased copper demands. Close monitoring by healthcare professionals is essential during pregnancy.
5. Can I have a normal life with Wilson’s disease?
With proper management, including medication, dietary adjustments, and regular medical follow-ups, individuals with Wilson’s disease can lead fulfilling lives and effectively control their symptoms.
Conclusion: Wilson’s disease is a complex genetic disorder that requires lifelong management. Early diagnosis, proper treatment, adherence to dietary modifications, and regular medical follow-ups are essential for managing the symptoms, preventing complications, and maintaining a good quality of life. Consulting with healthcare professionals specialising in Wilson’s disease is crucial for accurate diagnosis, treatment, and ongoing care.