Hepatorenal Syndrome: Causes, Symptoms, and Diagnosis
Hepatorenal Syndrome (HRS) is a severe complication of advanced liver disease, characterised by developing kidney dysfunction in individuals with liver cirrhosis or fulminant hepatic failure. This condition poses a significant threat to the overall health and survival of affected individuals.
Symptoms
The symptoms of Hepatorenal Syndrome can vary depending on the severity of the condition. Common signs and symptoms include:
- Worsening of liver disease symptoms, such as jaundice, ascites (abdominal swelling due to fluid accumulation), and hepatic encephalopathy (mental confusion and disorientation).
- Decreased urine output or complete absence of urine (oliguria/anuria).
- Rapid weight gain or loss.
- Fatigue, weakness, and malaise.
- Oedema (swelling) in the legs and ankles.
- Confusion and altered mental status.
Causes
The leading cause of Hepatorenal Syndrome is the progressive decline in liver function. The liver plays a crucial role in maintaining the balance of various chemicals and hormones in the body, including those involved in kidney function. As liver disease progresses, the liver becomes unable to perform its normal functions, leading to alterations in renal blood flow and kidney dysfunction.
Diagnosis
Diagnosing Hepatorenal Syndrome requires a comprehensive evaluation of the patient’s medical history, physical examination, and laboratory tests. The following diagnostic approaches are commonly employed:
- Medical History: Detailed assessment of symptoms, previous liver disease, alcohol consumption, and medication history.
- Physical Examination: Examine the abdomen for signs of liver disease, such as an enlarged liver or ascites.
- Laboratory Tests: Blood tests to evaluate liver function, kidney function, and other parameters. These may include liver enzyme tests, creatinine levels, electrolyte balance, coagulation profile, and complete blood count (CBC).
- Imaging Studies: Abdominal ultrasound or computed tomography (CT) scan to assess liver and kidney abnormalities.
- Kidney Biopsy: In some instances, a kidney biopsy may be performed to rule out other causes of renal dysfunction.
Tests Management
Once diagnosed with Hepatorenal Syndrome, it is crucial to determine the severity and stage of the condition. This helps guide appropriate management strategies and treatment decisions. The primary methods for assessing the severity of HRS include:
- The Model for End-Stage Liver Disease (MELD) Score: This scoring system evaluates liver function, serum creatinine, and bilirubin levels to predict the three-month mortality risk.
- Child-Pugh Score: This scoring system assesses liver disease severity based on factors such as bilirubin levels, albumin levels, prothrombin time, and the presence of ascites and hepatic encephalopathy.
Treatment
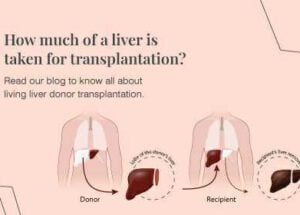
The definitive treatment for Hepatorenal Syndrome is liver transplantation. However, not all patients are suitable candidates for transplantation due to various factors such as age, coexisting medical conditions, and availability of donor organs. In such cases, treatment focuses on managing symptoms and slowing disease progression through lifestyle modifications, medication, and regular monitoring.
Prevention
Preventing the development or progression of Hepatorenal Syndrome involves effectively managing the underlying liver disease. This includes:
- Abstinence from Alcohol: If alcohol-related liver disease is the underlying cause, complete abstinence from alcohol is essential.
- Medication Adherence: Strict adherence to prescribed medications, particularly those aimed at controlling liver disease and preventing complications.
- Regular Medical Follow-up: Consistent monitoring of liver function, kidney function, and overall health through regular visits to a healthcare provider.
- Balanced Diet: Adopting a healthy, balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
- Vaccination: Ensuring up-to-date vaccinations, especially for hepatitis A and B, to prevent further liver damage.
When and Whom to Consult?
If you experience any symptoms suggestive of liver disease or kidney dysfunction, it is essential to consult a healthcare professional promptly. Additionally, individuals with known liver disease or those at risk should regularly consult their hepatologist or gastroenterologist for routine check-ups and appropriate management.
Summary
Hepatorenal Syndrome is a severe condition that requires early recognition and appropriate management to improve patient outcomes. Prompt diagnosis, understanding the causes and symptoms, implementing suitable treatment strategies, and preventing further complications are vital in managing this complex disorder. By focusing on comprehensive care and regular monitoring, healthcare providers can help individuals with Hepatorenal Syndrome achieve an improved quality of life and potentially extend their survival.
People also ask
1. What is the main cause of hepatorenal syndrome?
The main cause of hepatorenal syndrome (HRS) is the progressive decline in liver function. HRS typically occurs in individuals with advanced liver disease, such as liver cirrhosis or fulminant hepatic failure. The liver disease leads to alterations in renal blood flow and kidney dysfunction, resulting in HRS development.
2. What are the signs and symptoms of hepatorenal syndrome?
The signs and symptoms of hepatorenal syndrome can vary depending on the severity of the condition. Common manifestations include:
- Worsening of liver disease symptoms, such as jaundice (yellowing of the skin and eyes), ascites (abdominal swelling due to fluid accumulation), and hepatic encephalopathy (mental confusion and disorientation).
- Decreased urine output or complete absence of urine (oliguria/anuria).
- Rapid weight gain or weight loss.
- Fatigue, weakness, and malaise.
- Edema (swelling) in the legs and ankles.
- Confusion and altered mental status.
It’s important to note that these symptoms may overlap with those of advanced liver disease, making the diagnosis of HRS challenging.
3. What is the pathophysiology of hepatorenal syndrome?
The pathophysiology of hepatorenal syndrome is multifactorial and involves complex interactions between the liver, kidneys, and various regulatory systems in the body. The primary mechanisms underlying HRS include:
- Splanchnic Vasodilation: In liver disease, there is increased production of vasodilatory substances, such as nitric oxide, within the splanchnic circulation (blood vessels supplying the abdominal organs). This leads to the dilation of blood vessels and reduced blood flow to the kidneys.
- Renal Vasoconstriction: As a compensatory response to reduced blood flow, the kidneys undergo vasoconstriction (narrowing blood vessels) to maintain blood pressure. However, this adaptive mechanism results in inadequate renal perfusion and compromised kidney function.
- Fluid Redistribution: In advanced liver disease, fluid accumulates in the abdominal cavity (ascites) and lower extremities due to increased pressure in the portal vein system. This leads to decreased effective blood volume, further worsening kidney function.
These complex interactions contribute to the development of HRS, which is characterised by renal dysfunction in the setting of liver disease.
It’s essential to consult a healthcare professional for a thorough evaluation if you suspect hepatorenal syndrome or have any concerns about your health.