For those with Acute Liver Failure, undergoing a liver transplant is often the sole life-saving treatment available. The majority of organ allocation systems worldwide qualify these individuals for immediate liver transplants. The survival rate for patients with Acute Liver Failure has increased from less than 20% to 80% since the availability of this surgery.
The sudden onset of severe liver function failure is called Acute Liver Failure (ALF). Acute liver failure is rarer than chronic liver failure, which progresses gradually over time. In India, the most common cause of ALF is viral infection due to the hepatitis viruses. Other causes of ALF include:
- Overdose of paracetamol
- Ingesting toxic substances, such as phosphorus compounds (found in rat killer poison)
- Autoimmune hepatitis and Wilson’s disease.
Signs & Symptoms
Possible signs and symptoms of acute liver failure include:
- Jaundice (Yellowing of your skin and eyeballs)
- Pain in your upper right abdomen
- Abdominal swelling
- Nausea and Vomiting
- A general sense of feeling unwell (malaise)
- Disorientation or confusion
- Sleepiness
- Bleeding problems
Causes
Acute liver failure arises when the liver sustains severe cell damage, leading to a sudden loss of its ability to perform essential functions. Although many cases of acute liver failure have no detectable cause. A few potential causes include:
- Significant damage to the liver cells renders them incapable of functioning, leading to acute liver failure. A few potential causes include
- Hepatitis A, B, and E. Acute liver failure can also be brought on by the Epstein-Barr virus, cytomegalovirus, and herpes simplex virus.
- Acute liver failure can occur from taking more paracetamol than is advised for many days.
- Antibiotics, nonsteroidal anti-inflammatory medicines, and anticonvulsants are a few examples of prescription pharmaceuticals that might induce sudden liver failure.
- Abrupt liver failure has been associated with several herbal supplements and medicines.
- Certain toxins, such as Amanita phalloides, found in poisonous mushrooms, and carbon tetrachloride, an industrial chemical used as a refrigerant and solvent for waxes, varnishes, and other products, are known to cause liver damage.
- The disease known as autoimmune hepatitis occurs when the immune system of your body targets the liver cells, causing inflammation and damage. Liver failure may develop as a result.
- Acute liver failure can be brought on by vascular anomalies such as Budd-Chiari syndrome, which can obstruct the liver’s veins.
- Acute liver failure is associated with rare metabolic disorders, including acute fatty liver in pregnancy and Wilson’s disease.
- Liver failure may result from cancer that starts in or spreads to the liver.
- Liver failure can also result from major disruption of blood supply to the liver caused by shock and overwhelming infection (sepsis).
Complications
Acute liver failure often causes complications, including:
- Fluid build-up in the brain causes Cerebral oedema.
- Insufficient production of clotting factors by a failing liver makes blood thinner and more difficult to clot. This disease often results in gastrointestinal bleeding, which can cause bleeding disorders.
- The risk of infection is increased by acute liver failure, particularly in the respiratory, urinary, and blood systems.
- In many cases, kidney failure follows liver failure, particularly if you overdosed on paracetamol, which harms both your kidneys and liver.
Prevention
By caring for your liver, you can lower your risk of developing acute liver failure.
- Let your doctor know about all of your medications, including herbal and over-the-counter ones that can conflict with prescribed medicines.
- If you drink alcohol, do so sparingly. Avoiding alcohol or drinking very little is advisable.
- It’s important to protect your health by avoiding risky behaviours. Never share needles or use illegal intravenous drugs. Practice safe sex by using condoms. If you’re getting a tattoo or body piercing, choose a reputable, hygienic studio. It is also vital to avoid smoking to safeguard your overall well-being.
- Practice safe sex by using condoms. If you’re getting a tattoo or body piercing, choose a reputable, hygienic studio. It is also vital to avoid smoking to safeguard your overall well-being.
- If you have a history of hepatitis infection of any kind, chronic liver disease, or an elevated risk of contracting hepatitis, get vaccinated. Consult your physician about receiving the hepatitis B vaccine. Hepatitis A can also be prevented using a vaccination.
- Stay away from exposure to contaminated blood and bodily fluids. Hepatitis viruses can be transferred by accidental needle jabs or by not properly cleaning up bodily fluids or blood. Infections can also spread by sharing the same toothbrush or razor blades.
- Be cautious with aerosol sprays. Wear a mask or make sure the space is ventilated before using an aerosol cleaner. Similar precautions should be used when applying paint, fungicides, insecticides, and other hazardous substances. Follow product instructions carefully.
- Use gloves, long sleeves, a hat, and a mask to protect your skin when handling pesticides and other harmful chemicals.
- Maintain a healthy weight. Excess body weight can cause non-alcoholic fatty liver disease, a condition that may progress to fatty liver, hepatitis, or cirrhosis.
Diagnosis
Acute liver failure is diagnosed using the following tests and procedures:
- Blood Tests: Liver function is evaluated through specific blood tests. The time it takes for your blood to clot is determined by a prothrombin time test. Acute liver failure causes blood to clot more slowly.
- Imaging Tests: Your doctor may offer an ultrasound check to examine your liver. These tests can reveal liver damage and assist your doctor in determining the root cause of your liver condition. To get a clearer view of your liver and blood vessels, your doctor might recommend imaging tests like an abdominal CT scan or an MRI. Such tests can help pinpoint the underlying causes of acute liver failure, including liver tumors or Budd-Chiari syndrome. If your doctor suspects something but the ultrasound test comes back negative, they might be used.
- Liver Tissue Examination: A liver biopsy, which involves taking a small sample of liver tissue, may be suggested by your doctor. Your doctor might better understand why your liver is failing if you do this. A transjugular liver biopsy may be performed by the physician since patients with acute liver failure are susceptible to hemorrhage during the procedure. Following a small incision on the right side of your neck, the doctor inserts a thin tube called a catheter into a neck vein, which then passes through your heart and reaches your liver. After that, your physician takes a sample of liver tissue by passing a needle through the catheter.
Treatment
For the best chance of recovery, patients with acute liver failure must be promptly transferred to a hospital equipped with liver transplant facilities. While some patients can be treated with medicines alone, it is rare. Patients with Acute Liver Failure require intensive care from liver specialists. Patients who meet specific blood test criteria require a liver transplantation immediately because they will not be able to survive with standard medical care. In such cases, a timely liver transplant from either a living or deceased donor can be life-saving.
Acute liver failure treatments may include:
- Acetylcysteine is a medication commonly used to treat acute liver failure resulting from a paracetamol overdose. Other causes of acute liver failure may also be treated with this drug. Medications that neutralize toxins and reduce liver damage may also be used to treat poisonings caused by mushrooms and other toxic substances.
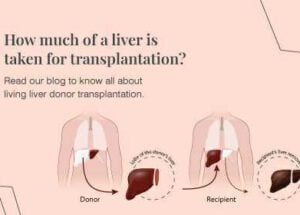
- The only option for treating acute liver failure that cannot be reversed is a liver transplant. A liver transplant involves surgically removing the failing liver and substituting it with a healthy liver from a donor. Along with trying to prevent problems from acute liver failure, your doctor will also try to manage the symptoms and indicators you are experiencing. Your care may include:
- Acute liver failure may result in cerebral oedema, where fluid buildup in the brain leads to increased pressure within the skull.
- Your care team will periodically collect blood and urine samples to monitor for potential infections. If an infection is identified or suspected, appropriate treatment will be initiated promptly.
- To reduce the chance of bleeding, doctors may administer specific medications. In cases of significant blood loss, diagnostic tests will be conducted to locate and address the source.
- You may require blood transfusions.
- Other organs like the kidneys and the heart may need to be supported with sophisticated devices till the patient recovers.