What is Liver Parenchymal Disease
August 17, 2023
What is a Liver Parenchymal Disease?
Liver Parenchymal Disease includes a variety of liver conditions affecting its functional tissue. These diseases stem from factors like viruses, alcohol, metabolic disorders, or autoimmune reactions. They can harm liver functions like detoxification and metabolism. Timely diagnosis and care are vital for managing these conditions and preserving liver health.
Table of Contents
- What is a Liver Parenchymal Disease?
- Causes of Liver Parenchymal Disease
- Symptoms of Liver Parenchymal Disease
- Types of Liver Parenchymal Diseases
- Treatment of Liver Parenchymal Diseases
- Prevention of Liver Parenchymal Diseases
- Conclusion
- Frequently Asked Questions
Causes of Liver Parenchymal Disease
We will explore the various factors and conditions that can lead to liver parenchymal disease.
-
Viral Infections
Hepatitis B and C infections can lead to liver inflammation, causing liver parenchymal disease. Chronic hepatitis C may progress to cirrhosis and parenchymal damage. Hepatitis A, while usually milder, can still result in liver inflammation in certain cases.
-
Alcohol Consumption
Excessive and prolonged alcohol consumption can lead to alcoholic liver disease, which damages the livers parenchymal cells. Conditions like alcoholic hepatitis and alcoholic cirrhosis can develop as a result.
-
Non-Alcoholic Fatty Liver Disease
NAFLD is a condition characterised by the accumulation of fat in the liver, not associated with excessive alcohol intake. It can progress to non alcoholic steatohepatitis, causing inflammation and damage to the liver parenchyma.
-
Autoimmune Conditions
Autoimmune liver diseases like autoimmune hepatitis can lead to chronic inflammation and damage to liver tissue, affecting the liver parenchyma.
-
Metabolic Disorders
Metabolic conditions such as hemochromatosis and Wilson’s disease can result in liver damage, impacting the liver parenchyma.
-
Vascular Disorders
Vascular disorders affecting blood flow to the liver can lead to liver parenchymal disease. Conditions like Budd Chiari syndrome, characterised by blood clotting in the liver’s veins, can result in liver damage.
-
Wilson’s Disease
Wilsons disease is an genetic condition that results in the buildup of copper, in the liver resulting in damage, to liver cells and impaired liver function.
-
Hemochromatosis
Hemochromatosis is a genetic disorder that causes excessive iron absorption and accumulation in the liver, resulting in parenchymal damage.
-
Other Factors
Severe malnutrition, chronic congestive heart failure and chronic renal failure can indirectly impact liver parenchyma by affecting overall health and liver blood flow.
Infections such as schistosomiasis can lead to liver parenchymal disease in regions where the disease is endemic.
Liver parenchymal disease has various causes, including viral infections, alcohol use, metabolic disorders, autoimmune conditions, vascular issues and genetics. Early diagnosis and suitable interventions, like lifestyle changes and medical treatments can prevent further liver damage. Maintaining a healthy lifestyle and undergoing regular medical checkups are crucial in managing and preventing liver parenchymal diseases and improving overall well being.
Symptoms of Liver Parenchymal Disease
Liver parenchymal disease presents diverse symptoms, depending on its cause and stage, warranting prompt medical evaluation. Common symptoms include jaundice, fatigue, abdominal discomfort, unexplained weight loss and more.
- Jaundice (yellowing of the skin and eyes)
- Fatigue and weakness
- Abdominal pain or discomfort
- Unexplained weight loss
- Swelling in the abdomen or legs (edema)
- Nausea and vomiting
- Loss of appetite
- Dark urine
- Pale-colored stools
- Itchy skin
- Enlarged spleen (splenomegaly)
- Confusion or changes in mental function
- Easy bruising and bleeding
- Spider-like blood vessels on the skin (spider angiomas)
- Fluid retention in the abdomen (ascites)
- Muscle wasting
- Fever and chills (in cases of infection)
- Elevated liver enzymes in blood tests
If you encounter any of these symptoms, especially if they persist for an extended period of time, it is critical that you get a medical assessment and diagnosis to determine the reason and proper therapy.
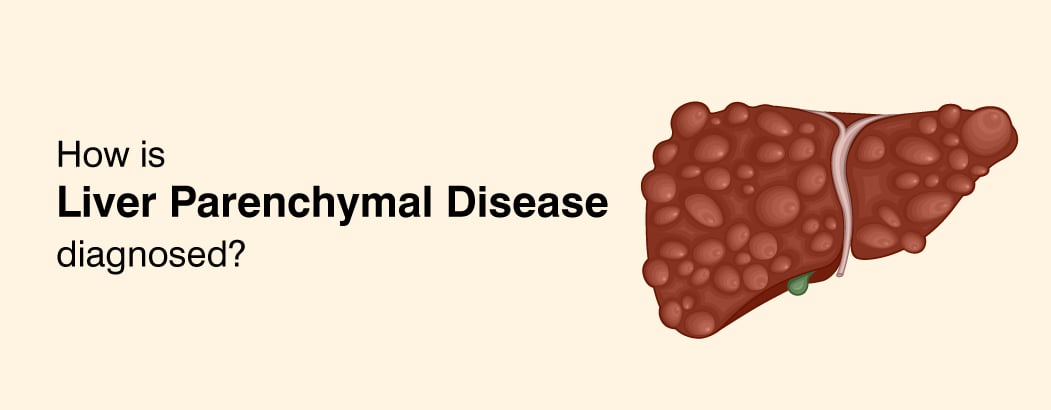
Types of Liver Parenchymal Diseases
Liver parenchymal illnesses are a diverse group of conditions, each with its own set of origins, symptoms, and treatment options. Some examples of frequent types are:
- Hepatitis: Inflammation of the liver caused by viral infections (Hepatitis A, B, C, and so on).
- Cirrhosis is a type of advanced scarring of the liver tissue that is commonly induced by chronic alcohol consumption or hepatitis.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Fat accumulation in the liver that is not caused by alcohol consumption and is connected with obesity and metabolic syndrome.
- Autoimmune Hepatitis: An immune system illness that causes inflammation and damage to liver cells.
- Hemochromatosis is the accumulation of too much iron in the liver, which can cause damage and dysfunction.
- Wilson’s Disease is a rare hereditary condition in which copper accumulates in the liver and other organs.
- Alcoholic Liver Disease: Liver damage induced by excessive alcohol consumption.
- Primary Biliary Cholangitis (PBC) is an autoimmune disease that affects the bile ducts of the liver.
- Primary Sclerosing Cholangitis (PSC) is characterized by chronic inflammation and scarring of the bile ducts located outside the liver.
- Liver Cancer: Primary liver cancer or malignancies that have spread to the liver.
- Drug-Induced Liver Injury: Liver damage caused by drugs or poisons.
- Alagille Syndrome is a hereditary condition that affects the bile ducts of the liver, causing liver and other health problems.
- Alpha-1 Antitrypsin Deficiency: A hereditary condition that can cause liver and lung difficulties.
- Hepatic Encephalopathy: Brain impairment caused by liver disease, which is frequently connected with cirrhosis.
- A pus-filled sac within the liver that is usually caused by infection.
- Hepatic steatosis is the accumulation of fat in liver cells, which is frequently related with obesity and metabolic disorders.
- Gilbert’s Syndrome is a harmless liver disorder that causes moderate jaundice.
- A noncancerous liver tumor made up of blood vessels is known as a hemangioma.
- Budd-Chiari Syndrome: A uncommon disorder characterized by hepatic vein obstruction.
- FNH (Focal Nodular Hyperplasia): A noncancerous liver tumor that can occur in some people.
It is vital to remember that these illnesses vary in severity and may necessitate distinct treatment techniques. To effectively treat liver parenchymal disorders, proper diagnosis and management are required.
Treatment of Liver Parenchymal Diseases
Treatment of Liver Parenchymal Diseases can involve a range of approaches depending on the specific condition and its causes. Here is a simplified overview:
- Lifestyle Modifications: Changes in lifestyle are critical for many liver disease. These may include eating a nutritious diet, exercising on a regular basis, decreasing weight and abstaining from alcohol or certain drugs.
- Antiviral Medications: In cases of viral hepatitis B and C antiviral drugs can help suppress viral activity and reduce liver inflammation.
- Immunosuppressants: Autoimmune liver diseases like autoimmune hepatitis may require medications that suppress the immune system’s activity to reduce liver inflammation.
- Managing Underlying Conditions: For liver diseases associated with metabolic issues like NAFLD or Hemochromatosis, managing the underlying condition is essential. This may involve managing diabetes, reducing iron levels, or addressing obesity.
- Cirrhosis Management: In advanced cases of cirrhosis treatment may involve managing complications like fluid retention, bleeding varices and hepatic encephalopathy. Liver transplants may be considered in severe cases.
- Bile Duct Conditions: For conditions affecting the bile ducts like PBC or PSC, medications can help manage symptoms and slow disease progression. In some cases, a liver transplant may be necessary.
- Cancer Treatment: Liver cancer treatment can include surgery, chemotherapy, radiation therapy, targeted therapies, depending on the stage and type of cancer.
- Genetic Disorders: Genetic liver conditions like Wilson’s Disease or Alpha-1 Antitrypsin Deficiency may require lifelong management with medications and dietary restrictions.
- Avoiding Toxins: For drug induced liver injuries, the primary treatment is discontinuing the offending medication or toxin.
- Regular Monitoring: Many liver diseases require ongoing monitoring through blood tests, imaging, and follow up appointments to assess treatment effectiveness and disease progression.
- Supportive Care: In some cases, supportive care measures like nutritional support and pain management are essential for maintaining quality of life.
- Preventive Measures: Preventive measures such as vaccination against hepatitis viruses and lifestyle changes to reduce risk factors can help prevent liver parenchymal diseases.
Remember, treatment plans are highly individualised and should be developed in consultation with a healthcare provider or liver specialist. Early diagnosis and prompt intervention can significantly improve outcomes for individuals with liver parenchymal diseases.
Prevention of Liver Parenchymal Disease
Prevention of Liver Parenchymal Diseases is crucial for maintaining liver health and reducing the risk of liver-related conditions. Here are simplified prevention measures:
- Vaccinations
- Safe Practices
- Moderate Alcohol Consumption
- Healthy Diet
- Maintain a Healthy Weight
- Regular Exercise
- Manage Medications
- Limit Toxin Exposure
- Screen for Liver Conditions
- Control Chronic Conditions
- Avoid High-Risk Behavior
- Limit Herbal Supplements
- Hepatitis C Testing
- Follow Medical Advice
- Liver-Friendly Lifestyle
Preventing liver parenchymal diseases requires a combination of vaccination, healthy living, risk reduction, and proactive healthcare. Consult with a healthcare provider for personalised guidance and screenings based on your individual risk factors and medical history.
Conclusion
Liver parenchymal disease covers a wide range of liver conditions caused by factors like infections, genetics, and metabolic issues. Identifying the root causes is crucial for management. Early diagnosis and tailored treatments can halt further liver damage. Preventing liver parenchymal diseases involves vaccinations, a healthy lifestyle, and regular check-ups for early detection.
Individuals with liver parenchymal diseases should seek timely medical care, make lifestyle changes and follow treatment plans to prevent liver damage. Early detection and personalised care are crucial for a better quality of life. Consult a liver specialist for guidance based on your needs and risks.
Frequently Asked Questions
-
Is liver parenchymal disease cirrhosis?
Liver parenchymal disease encompasses various liver conditions that affect the liver’s functional tissue called the parenchyma. Cirrhosis, however specifically denotes advanced liver scarring due to prolonged liver damage and inflammation. Although cirrhosis can result from some liver parenchymal diseases, the two terms differ with liver parenchymal disease being the broader classification.
-
What does liver parenchyma mean?
Liver parenchyma means the main working part of the liver, where important functions happen. It is made up of liver cells called hepatocytes and helps with tasks like filtering blood, making proteins and processing nutrients. When the liver parenchyma gets damaged, it can lead to liver problems.
-
Is liver parenchymal disease serious?
Yes, liver parenchymal disease can be serious. Its seriousness depends on factors like the underlying cause and disease stage. Early diagnosis and proper management are vital to reduce the severity and prevent complications such as cirrhosis or liver cancer.