HEPATITIS AND PREGNANCY
July 28, 2020
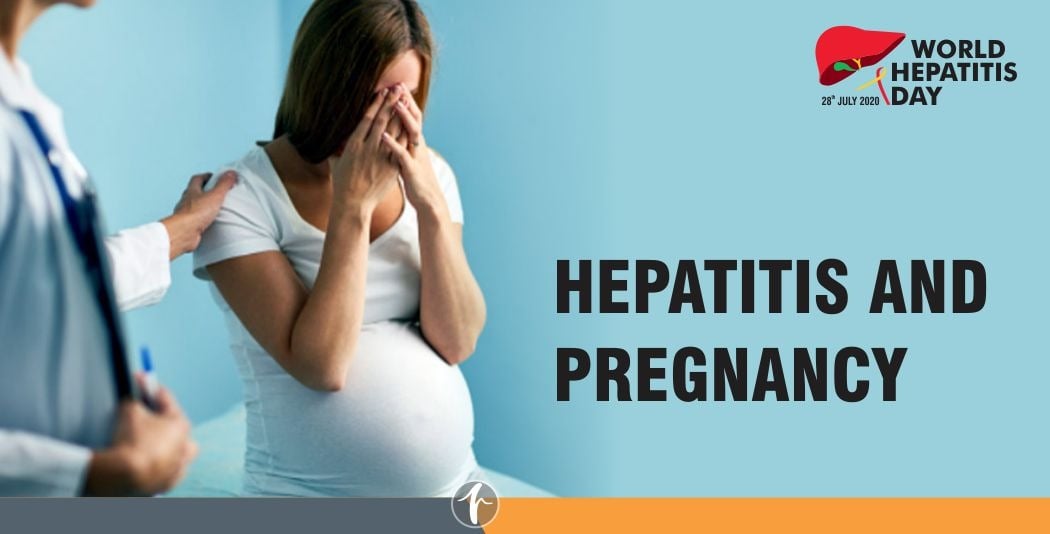
The inflammation of liver is called as Hepatitis. Usually the reason for hepatitis in general population is viral infection, alcohol, obesity, medications etc. Pregnancy is condition where immunity is very low so it is called as immunosuppressed state. That’s why chances of getting hepatitis in pregnancy are very high.
Acute viral Hepatitis:
Acute viral hepatitis is the most common cause for hepatitis in pregnancy. There are various viral infections that can affect the pregnancy like Hepatitis A (HAV), Hepatitis E (HEV), Hepatitis B (HBV), Hepatitis C (HCV) and rarely Herpes simplex virus (HSV). Pregnant women with acute hepatitis due to hepatitis E virus (HEV) or herpes simplex virus (HSV) have an increased risk of acute liver failure (a life threatening condition) compared to persons who are not pregnant.
Hepatitis A virus (HAV) infection does not progress to chronic infection, and HAV is generally transmitted via fecal-oral route; therefore, maternal-infant transmission is rare. The highest risk of gestational complications such as premature rupture of membrane, placental separation, or preterm labor is during the second half of pregnancy.
Similar to HAV Hepatitis E virus (HEV) also spreads through fecal-oral route or contaminated water. Acute hepatitis E is self-limiting in the vast majority of cases, but hepatitis E during pregnancy can cause severe hepatitis and acute liver failure, especially when it occurs in the third trimester. Maternal fatality of 16% to 20% had been reported when hepatitis E occurs in the third trimester of pregnancy and is caused by acute liver failure, eclampsia, or haemorrhage.
Chronic viral hepatitis:
Chronic viral hepatitis is more commonly seen in HBV and HCV infections. Usually these patients will be known case of underlying liver disease or incidentally diagnosed during routine evaluation in pregnancy. Sometimes these HBV and HCV chronic infections are notorious to transmit the virus to the infant / foetus if left untreated. The risk of vertical transmission (mother to child) of hepatitis viruses is higher in pregnant women with acute versus chronic infection. The diagnosis of HBV and HCV infection is crucial during pregnancy. All pregnant women should be tested for these viruses.
Risk of viral hepatitis in pregnant women:
| Type of viral hepatitis | Potential risk to mother | Timing of pregnancy with highest risk |
| Hepatitis A | Preterm labor | 2nd half of pregnancy, especially 3rd trimester |
| Hepatitis B | Flares of infection/Reactivation of virus | Can occur during pregnancy or postpartum period |
| Hepatitis C | None | |
| Hepatitis E | Acute liver failure/ Premature delivery / Hypertension | 2nd and 3rd trimester |
| HSV Hepatitis | Acute liver failure | 3rd trimester |
Similarly there is risk to foetus during and after the pregnancy. In the absence of prophylaxis, the risk of vertical transmission is up to 90% in case of HBV infection and 5 % in case of HCV infection. Children born to infected mothers may harbour infection throughout their life if not vaccinated at right time.
Preventive measures:
Hepatitis is best prevented. Avoid food and drink prepared under unhygienic conditions to avoid hepatitis A and E. Avoid sharing needles, razors and unprotected sex. If you are a health worker, handle blood, needles and medical equipment with care to prevent hepatitis B and hepatitis C. Early diagnosis and prevention is the key to manage hepatitis in pregnancy.
| Type of viral infection | Preventive measures |
| HAV | Vaccinate pregnant women who will be traveling to endemic areas |
| HBV | Passive/active prophylaxis. HBIG (Immunoglobulin) and HBV vaccination within 12 hours of birth for all new-borns of HBsAg mother |
| HCV | None / No Vaccine available |
| HEV | None/ No Vaccine available |