Carotid Endarterectomy (CEA): A Life-Saving Procedure to Prevent Stroke
April 10, 2025
Carotid endarterectomy (CEA) is a Neurosurgical procedure done to correct the stenosis(narrowing) of the Internal Carotid Artery(Chief blood supply) to the brain to reduce the risk of ischemic stroke of the brain.
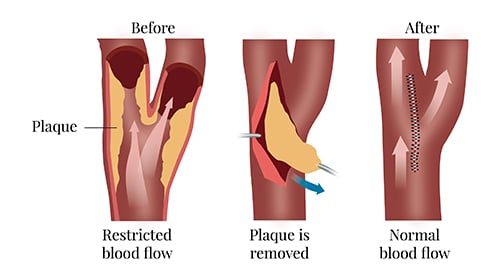
It is a surgery done in the neck at the bifurcation of the common carotid artery, where the main blood supply to the brain (the Internal carotid artery) originates. The artery is opened at the area of stenosis, and the atherosclerotic plaque is completely removed. The artery is then closed with fine sutures. The results were very good if this procedure was done under high magnification in Modern Neuromicroscopes.
What is Carotid Endarterectomy
Carotid endarterectomy is a procedure to treat carotid artery disease. This disease occurs when fatty, waxy deposits build up in one of the carotid arteries. The carotid arteries are blood vessels located on each side of the neck.
This buildup of plaque may restrict blood flow to your brain. Removing plaque causing the narrowing in the artery can improve blood flow in your carotid artery and reduce your risk of stroke.
In carotid endarterectomy, you receive a local or general anaesthetic. The surgeon makes an incision along the front of the neck, opens the carotid artery, and removes the plaques that are clogging the artery. Then, your surgeon repairs the artery with stitches or a patch made with a vein or artificial material (patch graft).
Sometimes, surgeons may use another technique called eversion carotid endarterectomy. This involves cutting the carotid artery and turning it inside out, then removing the plaque. Your surgeon then reattaches the artery.
Why and When Carotid Endarterectomy is Done
The most common cause of carotid artery stenosis is atherosclerosis, which causes plaque to form within the wall of the carotid artery. Generally, it is an age-related degenerative change, and other non-modifiable risk factors like Type II Diabetes and Hypertension can aggravate the disease process. Smoking, alcohol consumption, and obesity are modifiable risk factors that aggravate the progression of atherosclerotic changes and thus cause Carotid Artery Stenosis.
With the reduction of the calibre of the major blood vessels that supply to the brain the demand for oxygen supply to the brain decreases. When the stenosis is less it can cause temporary symptoms like transient ischemic attacks (TIA) of the brain, spinal cord and retina and is often the early indicator before a Major brain stroke.
The North American Symptomatic Carotid Endarterectomy Trial (NASCET) found that patients who have symptoms of stroke and high-grade Carotid stenosis (>70% block) significantly benefit from this surgery, and there is an almost 17% decrease in major brain strokes and a 7% decrease in deaths due to major strokes. European Carotid Surgery trial (ECT), Asymptomatic Carotid Atherosclerosis Study (ACAS), and many other major trials have established the usefulness of this surgery.
National Institute for Health and Clinical Excellence (NICE) guidelines recommend patients with moderate to severe (50–99% blockage) stenosis, and symptoms should undergo treatment at the earliest.
How to Get Ready for a Carotid Endarterectomy
Before the procedure, your healthcare provider will walk you through the details and give you an opportunity to ask any questions. You’ll be asked to sign a consent form, so be sure to read it carefully and clarify anything that’s unclear.
A complete medical evaluation will be conducted to confirm you’re fit for surgery. This may include a physical exam, blood work, and other diagnostic tests. Let your provider know about any allergies or sensitivities, especially to medications, latex, iodine, anesthesia, tape, or contrast dyes.
It’s important to inform your healthcare team about all medications and supplements you’re currently using, including prescription drugs, over-the-counter remedies, and herbal products. If you have a history of bleeding issues or are taking blood thinners like aspirin or anticoagulants, you might need to stop them temporarily as advised.
If you’re pregnant or suspect you could be, notify your provider in advance. You’ll likely be instructed to avoid eating or drinking for a certain time before surgery. A blood test might be done to check your clotting time.
You may be given a sedative before the procedure to help you relax. If you have a pacemaker, let your provider know.
If you smoke, it’s strongly recommended to quit before the operation. Doing so can support a smoother recovery and improve your overall health. Smoking increases the risk of blood clots and other complications.
Depending on your specific health needs, your provider may offer additional guidance to help you prepare for surgery.
Steps
Below is a step-by-step overview of how the carotid endarterectomy procedure is typically performed, from diagnosis to completion.
Step 1
Carotid endarterectomy is an operation during which the surgeon removes the fatty deposits to correct the narrowing and to allow blood and oxygen to flow freely to the brain.
Step 2
These two main arteries, one on each side of the neck, deliver blood and oxygen to the brain.
Step 3
Plaque builds up in large- and medium-sized arteries as people get older, more in some people than others depending on lifestyle and hereditary factors.
Step 4
This build-up is a vascular disease called atherosclerosis, or hardening of the arteries.
Step 5
The procedure takes about 2 hours to perform but may seem slightly longer depending upon the anesthetic and preparation time. For carotid endarterectomy, a general anaesthetic or a local anaesthetic (to numb the neck area) may be used.
Diagnosis
- If people remain awake during the Carotid endarterectomy operation, the surgeon can better evaluate how the brain is functioning.
- The surgeon makes an incision in the neck over the area of the artery that contains the blockage and an incision in the artery. The blockage is removed, and the incisions are closed. For a few days afterward, the neck may hurt, and swallowing may be difficult. Most people can stay in the hospital for 1 or 2 days.
Risk Factors
While carotid endarterectomy (CEA) is a commonly performed procedure to reduce the risk of stroke, several factors can influence the likelihood of complications both during and after surgery. Patient-specific conditions, the surgeon’s experience, and how well the surgery is managed before and after all play a role in the potential for adverse outcomes.
Some individuals may face a higher risk of cardiovascular events, such as heart attack or stroke, around the time of the procedure. Others might experience temporary or permanent nerve-related issues, especially affecting areas controlled by the cranial nerves, including movement of the face, tongue, or throat. Swelling near the surgical site may lead to bleeding or, in rare cases, affect breathing.
Additional risks can include infection, irregular heart rhythms, high blood pressure, or bleeding in or around the brain. Some patients may also experience seizures or temporary neurological symptoms like transient ischemic attacks (TIAs). The artery may become narrowed again over time, or similar issues may develop on the opposite side of the neck.
It’s important to consider allergies to medications or materials used during surgery, and pre-existing kidney problems should also be disclosed, as they may influence the surgical approach or recovery.
Frequently Asked Questions
1. Is carotid endarterectomy major or minor surgery?
Most studies on outcomes of carotid endarterectomy (CEA) have focused on the major complications of death and stroke. Less is known about minor but more common surgical complications such as hematoma, cranial nerve palsy, and wound infection.
2. What is the recovery time for carotid endarterectomy?
Most people will be able to return to work 3 to 4 weeks after having a carotid endarterectomy. The surgeon or general physician will be able to advise you further about returning to work. Being active can help your recovery, but you shouldn’t overdo it.
3. What is a common postoperative complication of carotid artery disease?
Postoperative complications of CEA include myocardial infarction, perioperative stroke, postoperative bleeding, and the potential consequences of cervical hematoma, nerve injury, infection, and carotid restenosis.
4. What do you monitor post carotid endarterectomy?
Postoperative care should include monitoring of the patient’s neurologic status, blood pressure control, and wound observation for hematoma.
5. What is the success rate of carotid artery surgery?
A carotid procedure may reduce the long-term risk of stroke from 2% per year to 1% per year. A procedure is most likely to benefit people who have 60% to 70% or more narrowing of the carotid arteries.







