Stress Urinary Incontinence: Causes, Treatments, and Prevention
April 18, 2025
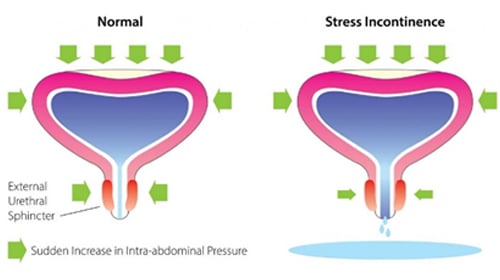
It is the complaint of involuntary leakage of urine during coughing, sneezing, or any other strain, such as lifting a weight. Stress incontinence is usually the result of the weakening of or damage to the muscles used to prevent urination, such as the pelvic floor muscles and the urethral sphincter. Occasionally, a patient will have frequency of urination and urgency only, but the stress leak will be detected by the urologist or gynaecologist on examination. Unless associated stress leak is treated, urgency or urge leakage may not be cured.
Causes
These problems may be caused by damage during childbirth, increased pressure on your tummy for example, because you are pregnant or obese, damage to the bladder or nearby area during surgery such as hysterectomy or neurological conditions that affect the brain and spinal cord, such as Parkinson’s disease or multiple sclerosis and certain medications.
Diagnosis
The diagnosis of Stress Urinary Incontinence (SUI) typically starts with a thorough discussion between you and your healthcare provider. Your healthcare provider will begin by evaluating your health background, discussing your typical urinary habits, and carrying out a physical exam to pinpoint the cause of your symptoms. For women, this may involve examining the abdomen, pelvic organs, and rectum, while for men, it may include an abdominal, prostate, and rectal exam.
A bladder diary may be recommended before your visit. This simple tracking tool records your fluid intake, urination times, leakage episodes, and related activities, providing valuable insights into your condition.
Depending on the case, your provider may perform or order additional tests, such as:
- A urinalysis is conducted to check for infections or blood in the urine, which could indicate other urinary tract problems.
- Bladder scan or ultrasound to check how much urine remains in your bladder after urination.
- The urinary pad test, where absorbent pads are weighed to estimate the volume of leakage.
- Cystoscopy uses a small scope to visually inspect the bladder and urethra for abnormalities.
- Urodynamic tests, which measure bladder pressure, urine flow, and muscle strength to assess how well the bladder and urethra function during storage and release of urine.
These evaluations help confirm the presence of stress incontinence and rule out other underlying conditions. In some cases, especially if surgery is being considered, more advanced testing may be needed to guide treatment decisions.
What are the Treatments Available?
Lifestyle changes such as losing weight and cutting down on caffeine, altering how much fluid you drink a day, and reducing alcohol consumption. Pelvic floor exercises – exercising your pelvic floor muscles by squeezing them, taught by a specialist.
Surgical Management
We at Dr Rela Hospital offer all the treatments aimed at curing stress Incontinence.
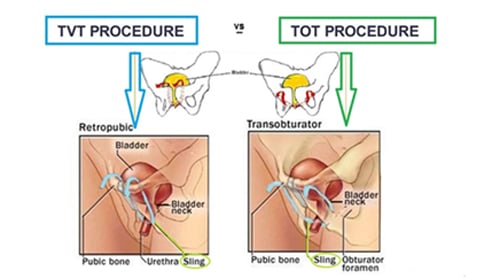
Mid-urethral Tapes
Tape is a thin strip of surgical mesh inserted through cuts (incisions) inside the vagina and groin or lower abdomen, and threading the tape behind the tube that carries urine out of the body (urethra).
The sling can be made of:
- Tissue taken from another part of your body (autologous sling) – from the thigh or the abdominal wall.
- Polypropylene meshes – These can be fitted from thigh to thigh (TOT or TVT-O) or from the lower abdomen (TVT)
Colposuspension
Colposuspension involves making an incision in your lower abdomen, lifting up the neck of your bladder, and stitching it in this lifted position. This can be done either by open operation- open colposuspension, or by laparoscopic (keyhole) colposuspension, where surgery is carried out through one or more small incisions. We at Dr Rela Hospital offer both procedures.
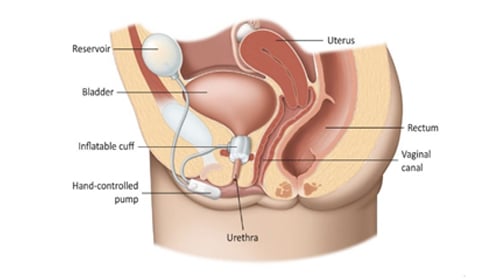
Artificial Urinary Sphincter
In severe cases or if you have had previous surgery for stress incontinence, it may be suggested that you have an artificial urinary sphincter fitted. An artificial sphincter consists of 3 parts:
- A circular cuff that is placed around the urethra – this can be filled with fluid when necessary to compress the urethra and prevent urine from passing through it.
- A small pump that contains the mechanism for controlling the flow of fluid to and from the cuff.
- A small fluid-filled reservoir in the abdomen – the fluid passes between this reservoir and the cuff as the device is activated and deactivated.
Lifestyle and Behavioral Strategies
Lifestyle modifications often play a key role in managing symptoms:
- Weight management: Losing excess body weight can reduce pressure on the bladder.
- Smoking cessation: Quitting helps reduce chronic coughing and irritation to the bladder.
- Bladder-friendly habits: Avoiding caffeine, alcohol, and spicy or acidic foods may help control urgency and frequency.
- Preventing constipation: A high-fiber diet and proper hydration can ease bowel function and minimize pressure on the bladder.
Bladder training or timed voiding may also be recommended. This involves scheduled bathroom visits to gradually increase the time between urinations, training the bladder to hold more urine over time.
Pelvic Floor Muscle Therapy
One of the most effective methods for reducing SUI is by strengthening the pelvic floor muscles.
- Kegel exercises: These target the muscles that support the bladder and urethra. Regular practice can significantly improve control over leakage.
- Biofeedback therapy: Sensors guide patients to ensure they’re activating the correct muscles.
- Pelvic floor physical therapy: Specialized therapists offer customized exercise routines and techniques.
- Vaginal cones (for women): These weighted devices are inserted into the vagina and held in place using pelvic muscles, enhancing strength over time.
Visible improvement from these exercises may take 4–6 weeks of consistent effort.
Complications
Stress urinary incontinence can affect more than just physical health; it can also influence emotional well-being, social interactions, and quality of life. People with this condition may experience embarrassment or self-consciousness due to the unpredictable nature of urine leakage. Over time, these emotions can lead to decreased social interaction, lower self-esteem, and in some cases, may trigger symptoms of anxiety or depression.
In addition to emotional distress, stress incontinence may lead to physical discomfort. Continuous skin contact with urine can cause irritation, rashes, or even skin breakdown if not managed properly. In more severe cases, individuals with limited mobility may develop pressure sores or be at increased risk for urinary tract infections due to prolonged moisture exposure.
For some, stress incontinence may coexist with other forms of urinary leakage, such as urgency incontinence, forming what is known as mixed urinary incontinence. This combination can further complicate symptom management.
Surgical treatments for stress incontinence, while often effective, also carry potential risks. Possible complications include discomfort, infections, bleeding, or unintentional harm to nearby organs like the bladder or intestines. In rare instances, materials used during surgery, such as slings or artificial sphincters, may erode or require further intervention. Postoperative issues like difficulty urinating or pain during sexual activity may also occur in some individuals.
In conclusion, the complications associated with stress urinary incontinence emphasize the need for early detection and holistic treatment to alleviate both physical and emotional challenges.
Conclusion
Stress urinary incontinence is a common yet often underreported condition that can significantly affect day-to-day comfort and confidence. Although it may seem daunting, the positive aspect is that numerous effective treatments and lifestyle adjustments are available, allowing many individuals to regain control and enhance their quality of life. What matters most is timely intervention and open communication with a healthcare provider. Early action not only helps in managing symptoms more effectively but also prevents complications down the road. By staying informed, proactive, and positive, patients can navigate this condition with dignity and hope.
Frequently Asked Questions
1. What is the difference between stress incontinence and urge incontinence?
Stress incontinence is caused by weak pelvic floor muscles or pressure on the abdomen, leading to small urine leaks during activities like coughing or lifting. Urge incontinence stems from bladder issues and causes sudden urges followed by larger urine leaks.
2. Can I prevent stress urinary incontinence?
Yes, stress urinary incontinence can often be prevented by maintaining a healthy weight, avoiding smoking, doing regular pelvic floor exercises (especially during pregnancy), and preventing constipation.