Osteoporosis: Causes, Symptoms, and Treatment
March 25, 2025
Osteoporosis, which means porous bones, weakens the bone structure and increases the risk of unexpected fractures. This condition reduces bone mass and strength, often developing silently without noticeable symptoms. Many people do not realize they have osteoporosis until a minor fall or a sudden movement like coughing or sneezing causes a fracture. The most commonly affected areas include the hip, wrist, and spine. A spinal vertebral fracture can lead to posture changes, a stooped appearance, or spinal curvature. Some individuals may also notice a decrease in height or a difference in how their clothing fits.
Causes
Bone remodelling, which occurs most frequently in young people, is the ongoing breakdown and replacement of bone in the body. A person’s bone mass typically peaks in their mid-to-late 20s. Bone loss occurs when bone breakdown outpaces bone growth, typically starting in the middle of a person’s 30s. Calcium, the mineral that gives bones their hardness, begins to be lost from bones quicker than it can be replaced. As a result, less bone remodelling occurs, which causes the bones to thin.
Risk Factors
Many people who have osteoporosis have several risk factors, but not everyone who has the disease does. Therefore, you may be able to change some risk factors, while you cannot change others. Nevertheless, you might be able to avoid sickness and fractures by being aware of these factors.
Your risk for osteoporosis could be affected by the following factors:
- Sex: If you are a woman, your risk of having osteoporosis is higher. This is because women have lower peak bone mass and smaller bones than men. Men are still at risk, though, particularly after 70.
- Age: Bone loss occurs more quickly, and new bone growth is slower as you age. As a result, your risk of osteoporosis can rise as your bones deteriorate over time.
- Body weight: Because they have less bone to lose than people with thicker bones, thin, slender women and men are more likely to develop osteoporosis.
- Family background: If one of your parents has experienced osteoporosis or a hip fracture, you may be more susceptible to fractures and osteoporosis.
- Hormonal changes: Your risk of developing osteoporosis may rise with low levels of specific hormones. For example, women’s low oestrogen levels following menopause.
- Low levels of oestrogen in premenopausal women can lead to abnormal lack of menstruation, brought on by hormone abnormalities or excessive physical exercise.
- Low testosterone levels in males. Osteoporosis is a danger for men with diseases that lower testosterone. But the progressive testosterone decline with age is probably not the main factor in bone loss.
- Diet: A diet deficient in vitamin D and calcium can raise your risk of osteoporosis and fractures from childhood into adulthood. Your risk of bone loss and osteoporosis may increase due to excessive dieting or inadequate protein intake.
- Lifestyle: Bone strength can be maintained by leading a healthy lifestyle.
- Low levels of physical activity and extended periods of inactivity can also speed up bone loss, among other factors. Additionally, they put you in poor physical shape, raising your risk of fracturing a bone if you fall.
- Osteoporosis is significantly increased by chronic high alcohol consumption.
- Smoking increases the risk of osteoporosis and fractures. Researchers are currently determining whether smoking’s adverse effects on bone health are due to tobacco usage alone or whether smokers are more likely to develop osteoporosis.
Signs and Symptoms
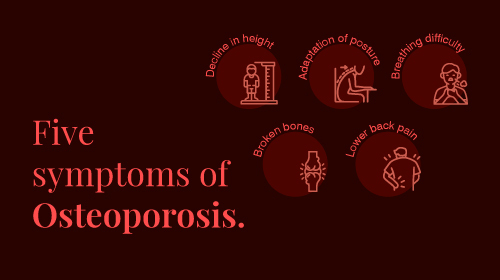
Osteoporosis typically shows no symptoms. It is sometimes referred to as a silent sickness for this reason. However, be on the lookout for the following:
- A decline in height (getting shorter by an inch or more)
- Adaptation of posture (stooping or bending forward)
- Difficulty breathing (smaller lung capacity due to compressed disks)
- Broken bones
- The lower back hurts
Diagnosis
Your doctor may conduct a test to find out about your bone mineral density (BMD). Dual-energy X-ray absorptiometry, often known as a DEXA or DXA scan, is another name for bone mineral density examinations. The strength of the spine, hip, and wrist bones can be examined using these X-rays, which emit very modest doses of radiation.
A bone density test ought to be performed on all women over the age of 65. For females who have osteoporosis risk factors, the DEXA scan may be completed sooner for females with osteoporosis risk factors. Consider obtaining a bone density test if you’re a man over 70 or younger with risk factors.
Treatment
Exercise, vitamin and mineral supplements, and medications are all possible treatments for osteoporosis that has already progressed. You may benefit from taking supplements and engaging in physical activity to avoid osteoporosis. Exercises, including weight bearing, resistance, and balance, are all crucial.
Eating a nutritious, balanced diet that contains the following foods is essential for treating osteoporosis:
- Consume plenty of fruits and vegetables.
- Make sure to take calories suitable for your age, height, and weight. Your doctor or health care provider can assist you in figuring out how many calories you need daily to stay healthy.
- Calcium, vitamin D, and protein-rich foods and drinks. These aid in reducing bone loss and preserving general health. Eating a diet high in all nutrients is crucial to safeguard and maintain bone health.
Lifestyle Changes to Follow
For the best possible bone health, a healthy diet and lifestyle are essential. You ought to:
- Stay away from secondhand smoke, and if you smoke, stop.
- Limit your alcohol consumption to one drink per day for women and two drinks per day for men.
- Ask your doctor about any factors, such as medications or other medical conditions, that could harm your bones or increase your risk of falling when you visit for routine checks.
Get a Sufficient Intake of Calcium and Vitamin D
Your bones can become brittle if you don’t get enough calcium or vitamin D. Adults up to 70 are advised by the National Institutes of Health to consume 600 IU of vitamin D daily. They require 800 IU of vitamin D per day after the age of 70. Women and men up to the age of 50 both need 1000 mg of calcium daily; therefore, 1200 mg of calcium per day is necessary for men and women over 50 and 70.
Frequently Asked Questions
1. When should you call the doctor about osteoporosis?
All women over 65 should have a bone density test performed and any younger women with an elevated risk of fracture. If they are older than 70 or have a high risk of developing weakened bones, men may wish to talk to their doctor about getting screened for osteoporosis.
2. What can you do if you are living with osteoporosis?
Limit alcohol intake, eat a calcium-rich diet with dairy and other sources, stay active with 30 minutes of weight-bearing exercise daily, and get enough vitamin D through safe sun exposure.
3. What are the early warning signs of osteoporosis?
A fractured or collapsed vertebra can cause back pain, height loss over time, and a hunched posture. Bones may also break more easily than expected.
4. What happens if you have osteoporosis?
Osteoporosis weakens bones, making them brittle and prone to fractures, even from minor actions like coughing or bending.







