Pericarditis: Causes, Symptoms, and Treatment
March 16, 2025
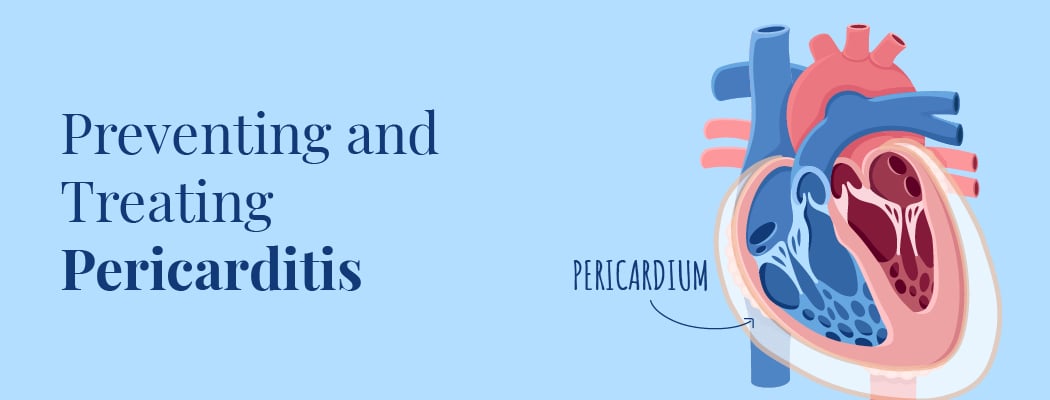
The pericardium is a thin, two-layered sac covering the heart’s outer surface. The heart pump helps to lubricate the heart, shields it from infection and malignancy, and keeps it in the chest wall. The pericardium becomes inflamed in the thin, two-layered, fluid-filled sac when you have pericarditis. The typical course of pericarditis is one of abrupt onset and may extend for a few weeks to a few months. However, the ailment typically goes away in three months. In addition, there can be fluid accumulation in the space between the pericardial layers, known as pericardial effusion. Pericarditis is a condition that affects anyone, but is most common in men aged 16 to 65.
Pericarditis typically starts quickly and lasts for a short time – this is known as acute pericarditis. However, if pericarditis lasts for an extended period, it is considered chronic pericarditis.
Types
- Acute pericarditis: Pericardial inflammation that appears out of the blue along with the development of symptoms.
- Chronic pericarditis: Pericardial inflammation that persists for at least three months following an acute incident.
- Constrictive pericarditis is a severe condition where the pericardium’s inflammatory layers stiffen, produce scar tissue, thicken, and adhere to one another. As a result, your heart’s regular operation is hampered by constrictive pericarditis. This typically occurs following a number of episodes of acute pericarditis over time.
- An infection, whether bacterial, fungal, viral, or parasitic, can cause an infectious form of pericarditis to manifest.
- Unknown causes of pericarditis are referred to as idiopathic pericarditis.
- Traumatic pericarditis manifests after a chest injury, such as that sustained in a vehicle accident.
- Uremic pericarditis occurs as a result of kidney failure.
- Malignant pericarditis is brought on by cancer that spreads throughout your body.
Pericarditis vs Myocarditis
The muscle of your heart has myocarditis. Your pericardium develops pericarditis. Viruses most frequently cause myocarditis and pericarditis. Both can cause chest pain, but the one caused by pericarditis should subside as you sit up and lean forward.
Quick Facts
These are some important pericarditis-related points.
- The pericardium, a sack-like tissue that houses the heart, swells when someone has pericarditis.
- Numerous factors, such as parasites, fungi, or bacterial or viral infections, might contribute to the illness.
- A virus typically brings on pericarditis.
- Palpitations, a dry cough, and shoulder soreness are pericarditis symptoms.
- Pericarditis can occasionally leave a lasting scar on the pericardium.
Who is Susceptible to Pericarditis?
Pericarditis can affect anyone, although it more frequently affects men and adults between the ages of 16 and 65 who were assigned male at birth. Pericarditis affects about 28 people out of every 100,000 people annually.
How Does My Body Respond to Pericarditis?
When you have pericarditis, the membrane surrounding your heart becomes inflamed and reddened, similar to the skin around a cut. The pericardium covers the outside of your heart and is a delicate, two-layered, fluid-filled sac. It keeps your heart lubricated, protects it from disease and cancer, and keeps your heart inside your chest wall. Additionally, it prevents your heart from overexpanding when blood volume rises, keeping your heart healthy.
Symptoms
Chest pain is a sign of pericarditis in about 85 to 90 percent of cases.
A sudden onset of a sharp or stabbing pain in your chest may feel like a heart attack. This is because the area behind your breastbone in your chest, either in the center or on the left, may be painful. In addition, your jaw, arms, shoulders, and neck could all experience pain.
Additional signs include:
- Fever, exhaustion, or weakness
- Breathing difficulties, mainly when lying down, and heart palpitations
- Swelling in your ankles, abdomen, feet, and legs due to a dry cough
Your symptoms might get worse if you:
- Lay flat
- Inhale deeply and swallow
Constrictive pericarditis may cause swelling in the feet, ankles, and legs and shortness of breath with exertion. The pericardium becomes thick or challenging in this type of severe pericarditis. When this occurs, the heart’s ability to expand is restricted, which prevents your heart from functioning normally. When your heart is constricted, blood can go back into your lungs, belly, and legs, causing oedema and congestive heart failure symptoms. Another potential condition is an aberrant cardiac rhythm.
Causes
The pericardium consists of two layers separated by a small amount of fluid. This fluid helps the two membranes move smoothly together. If the pericardium becomes infected and expands, the two layers of the pericardium will come into contact, causing friction.
In many cases, the primary cause of pericarditis cannot be identified. Pericarditis is an illness that is not understood and is known as idiopathic. Many cases are caused by viral infections that cannot be detected.
The following viruses are associated with acute pericarditis:
- Enteroviruses, including the common cold and viral meningitis
- HIV
- Glandular fever
- Herpes simplex
- Cytomegalovirus
- Adenoviruses, including pneumonia and bronchitis
- Influenza
- Hepatitis C
Pericarditis is often a complication that arises after a significant heart attack. This may be due to irritation of the heart muscles. It is a condition in which the pericardium becomes inflamed.
Pericarditis may develop weeks after a heart attack or operation, called Dressler’s syndrome. It is a disorder that affects the way your skin and hair grow. In this case, the cause may be autoimmunity.
Other causes of pericarditis include:
- Systemic inflammatory diseases, including rheumatoid arthritis or lupus
- Trauma
- Kidney failure
- Metabolic disorders, such as Gout
- Parasite
- Radiotherapy
- Fungi such as Histoplasmosis and Candida
- Underlying diseases such as AIDS, cancer, and tuberculosis
- Underactive thyroid
- Certain medications, including penicillin, warfarin, and phenytoin
Diagnosis
Two key indicators that you may have pericarditis and not a heart attack are chest pain with breathing and sharp pain in the back of your shoulders that feels better when you sit up and lean forward. Moreover, your doctor will question you about your symptoms, medical history, and any recent illnesses you may have had, as well as any heart ailments, surgeries, and other health issues that may increase your risk of developing pericarditis.
Your doctor will pay attention to your heart. The “pericardial rub” is a rubbing or creaking sound brought on by the friction of the irritated pericardium lining. Leaning forward, holding your breath, and exhaling will help them hear it the best.
Your doctor might also detect crackles in your lungs, which are indicators of fluid in the area around your lungs or additional liquid in your pericardium, depending on how severe the inflammation is.
Other diagnostic tests consist of the following:
- Chest X-ray, which reveals your heart’s shape and any excess fluid that may be present, and an electrocardiogram (ECG or EKG), which examines your heart’s rhythm.
- Using echocardiography, you may determine your heart’s size, shape, and presence of any fluid buildup.
- Right heart catheterization, which provides information about the filling pressure in your heart; CT and MRI images, which provide a thorough view of your pericardium; and blood tests to look for inflammation markers
Procedures
If medications are ineffective, a surgical option like pericardiocentesis may be considered. This procedure involves inserting a small tube into the pericardial cavity to drain excess fluid, which may be left in place for a few days to ensure complete drainage.
Pericardiectomy: Surgery may be done to remove the entire sac if the pericardium becomes particularly stiff and causes extra pressure on the heart. This is a risky procedure that is only used in cases of extreme need.
Prevention
Pericarditis, wildly viral pericarditis, cannot be wholly avoided.
Rest and stay out of any strenuous physical activities until you fully recover. How long you should restrict your exercise should be discussed with your doctor.
As soon as you notice any recurring symptoms, consult your doctor.
Primary care doctors, such as family doctors, internists, or pediatricians, often diagnose and treat pericarditis. Depending on the patient’s age and medical conditions, a cardiologist, pediatric cardiologist, or infectious disease specialist may be involved.
Frequently Asked Questions
1. Is pericarditis life-threatening?
Pericarditis can range from a non-life-threatening sickness to a superficial infection that goes away on its own. Poor heart function and fluid accumulation around the heart can exacerbate the disease. However, when pericarditis is treated quickly, the outcome is favorable. The majority of people heal in two to three months.
2. Will pericarditis go away?
Most of the time, mild cases of pericarditis resolve independently. Medications are commonly used to treat more severe cases, while surgery may be required in rare instances. Detecting and addressing pericarditis early can help reduce the risk of long-term complications.
3. Can the heart heal after pericarditis?
Certain cases might result in persistent pericarditis and other significant heart issues if left untreated. Pericarditis recovery can take weeks or even months. However, rest and regular treatment can help you fully recover and lower your chances of contracting it again.