Gangrene – Definition, Causes, Symptoms, and Treatment
March 27, 2025
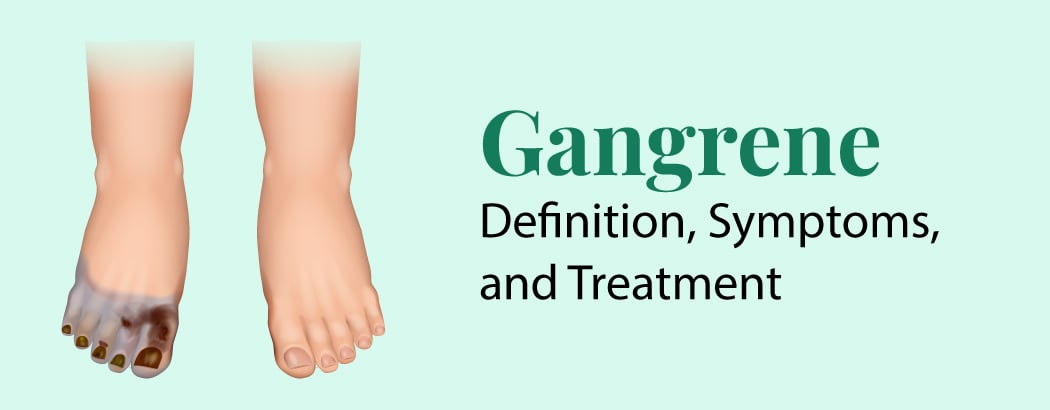
Gangrene is the death of bodily tissue brought on by a severe bacterial infection or a reduction in blood supply. It frequently affects the arms and legs, especially the toes and fingers. Gangrene can also affect the body’s internal organs, including the gallbladder and muscles. Antibiotics, oxygen therapy, and surgery to remove dead tissue and restore blood flow are among the possible treatments for gangrene. The chance of recovery from gangrene improves with prompt diagnosis and treatment.
What is Gangrene?
A major illness called gangrene causes a bodily component to start decomposing. This process is commonly described as necrosis or tissue death. A significant lack of blood flow to an extremity of the body, such as the hands, feet, nose, or ears, or an overpowering infection can result in gangrene.
Sepsis (blood infection) or total loss of the afflicted extremity are possible outcomes of gangrene. If left untreated, it can become life-threatening very quickly.
Types of Gangrene
Gangrene comes in several forms, each with unique causes and effects:
- Dry gangrene arises when blood flow to an area is restricted without infection. The affected skin remains dry, without blisters or pus. Atherosclerosis, recognized by plaque buildup in the arteries, is a common cause.
- Wet gangrene develops when poor circulation is combined with a bacterial infection. Blisters filled with pus form on the skin, giving it a “wet” appearance. This type spreads rapidly to surrounding tissues.
- Gas gangrene is a severe bacterial infection that destroys soft tissues and blood cells. The bacteria multiply quickly within muscle tissue, producing toxins and releasing gas. This condition progresses rapidly and can become life-threatening within hours.
- Fournier’s gangrene is a rare but serious bacterial infection that affects the genital area, primarily in males.
- Internal gangrene results from blocked blood flow to internal organs like the gallbladder, intestines, or appendix. For example, a gangrenous gallbladder can develop as a complication of chronic cholecystitis, where prolonged inflammation leads to tissue death.
- Meleney’s gangrene is a rare form of gangrene that typically develops as a complication after surgery. Painful skin lesions begin to appear within one to two weeks following the procedure. Also known as progressive bacterial synergistic gangrene, this condition requires medical attention to prevent further tissue damage.
Symptoms of Gangrene
Depending on the kind and intensity, gangrene can present with a variety of symptoms and clinical indications. Important gangrene warning indicators include:
- Skin Changes: Gangrenous tissue’s color, texture, and appearance frequently show noticeable changes. Dry gangrene may seem light or blueish-black, and wet or gas gangrene may appear dark red or greenish-black.
- Pain: Gangrenous tissue can cause pain, varying from a little soreness to an intense, stabbing ache. But occasionally, especially with diabetic neuropathy, people may feel less sensitivity or numbness in the afflicted area.
- Blisters and Ulceration: Blisters filled with pus or foul-smelling fluid may grow on the skin in wet gangrene. These blisters may burst and leave open sores or ulcers. These ulcers might be prone to infection and leak fluid.
- Bad Odour: Bacterial infection and tissue degradation in gangrene can produce an unpleasant stench that is typically compared to rotten or putrid. The smell is worse when the gangrene is damp.
- Lack of Sensation: People who have gangrene, particularly those who have diabetes or vascular disease, may feel numbness or loss of feeling in the affected area.
- Swelling and Tenderness: Inflammation and tissue necrosis can cause gangrenous regions to swell, feel painful to the touch, and become warm. Over the afflicted region, the skin may feel stretched out and constricted.
Diagnosis for Gangrene
- Blood Tests: An elevated white blood cell count often indicates an infection. Additional tests can detect specific bacteria and other germs.
- Fluid or Tissue Culture: A fluid sample from a skin blister is analyzed for bacteria, while a tissue sample is examined under a microscope for signs of cell death.
- Imaging Tests: X-rays, CT scans, and MRI scans provide detailed images of organs, blood vessels, and bones, helping determine how far gangrene has spread.
- Surgical Examination: A surgical procedure may be performed to assess the extent of tissue infection and gain a clearer view inside the body.
Treatment for Gangrene
Gangrene is often treated with one or more of the following techniques:
- Surgical Debridement: To stop gangrene from spreading and to speed up the healing of wounds, surgical debridement entails removing diseased or dead tissue. As much healthy tissue as possible is preserved during this surgery, with necrotic or diseased portions removed.
- Antibiotic Therapy: In situations of wet or gas gangrene, antibiotics are frequently administered to treat bacterial infections linked to gangrene. Intravenous use of broad-spectrum antibiotics can target a variety of microorganisms and avoid systemic illness.
- Dressing Changes: Managing gangrenous wounds, encouraging the growth of granulation tissue, and preventing infection all depend on proper wound care and dressing changes. In order to keep the wound moist and promote healing, wounds can be cleansed, debrided, and bandaged appropriately.
- Amputation: To remove the diseased limb or finger and stop the infection from spreading further, a surgical amputation may be required in severe cases of gangrene when there has been considerable and irreparable tissue destruction.
- Revascularization procedures: Angioplasty, stenting, or bypass surgery are examples of revascularization operations that may be carried out in situations of ischemia or arterial gangrene in order to salvage viable tissue and restore blood flow to the damaged area.
- Hyperbaric Oxygen Therapy: Hyperbaric Oxygen Therapy is a technique that enhances oxygen delivery to tissues and speeds up wound healing by inhaling pure oxygen within a pressurized chamber. For some forms of gangrene, such as diabetic foot ulcers or resistant wounds, hyperbaric oxygen therapy may be utilized as a secondary treatment.
Frequently Asked Questions
1. How long does wet gangrene take to cause death?
Wet gangrene is the most severe form, rapidly progressing to sepsis and potentially causing death within hours or days if not treated promptly.
2. What is the difference between gangrene and necrosis?
Necrosis describes the overall death of body tissue, whereas gangrene is a specific form of necrosis caused by restricted blood flow, often resulting in tissue decay.
3. Is gangrene contagious?
Gangrene itself is not contagious, but the bacteria responsible for certain types can spread through open wounds or contaminated medical equipment.
4. Is gangrene reversible?
Gangrene grows when your tissue dies due to a lack of blood supply. Once it develops, it cannot be reversed. However, early treatment can stop it from spreading and help preserve healthy tissue.