Gestational Diabetes
July 2, 2020

What is gestational diabetes?
Diabetes is a disease in which levels of glucose (sugar) in the bloodstream are higher than normal. Gestational diabetes is a form of diabetes that can develop during pregnancy, usually in the second trimester.
Glucose is produced in the body from the foods you eat. The pancreas, an organ located just behind the stomach, produces insulin. Insulin is a hormone that takes the glucose from the bloodstream and carries it inside your body’s cells where it is used for energy, as well as allowing excess glucose to be stored properly. During pregnancy, the placenta produces hormones that help the baby develop. These hormones also block the effects of insulin in the woman’s body, increasing her blood sugar levels. Most women who have gestational diabetes have no symptoms.
Who is at risk?
Gestational diabetes affects about 4–8 of every 100 pregnant women. The incidence rate is sometimes reported as 16% in Indian women. Any pregnant woman can develop the condition, but some women are at greater risk than others. Known risk factors include:
- Age (older than 25 years; the risk is even greater after age 35)
- Race (occurs more often in African Americans, Hispanics, American Indians, and Asian Americans)
- Overweight and obesity
- Personal history of gestational diabetes or prediabetes
- Having delivered a baby weighing more than 9 pounds
- Family history of type 2 diabetes (in parents or siblings)
Among women with these risk factors, as many as 14 in 100 develop gestational diabetes.
How do you know if you have gestational diabetes?
Most women with gestational diabetes have no warning signs or symptoms, so all pregnant women should be tested for this condition between the 24th and 28th weeks of pregnancy. For minority women who are obese and who have had a previous history of gestational diabetes or a family history of type 2 diabetes, experts recommend testing at the first prenatal visit. The test is called oral glucose tolerance test (OGTT) and involves measuring blood glucose levels both before and after drinking a sugary liquid.
Can gestational diabetes be dangerous?
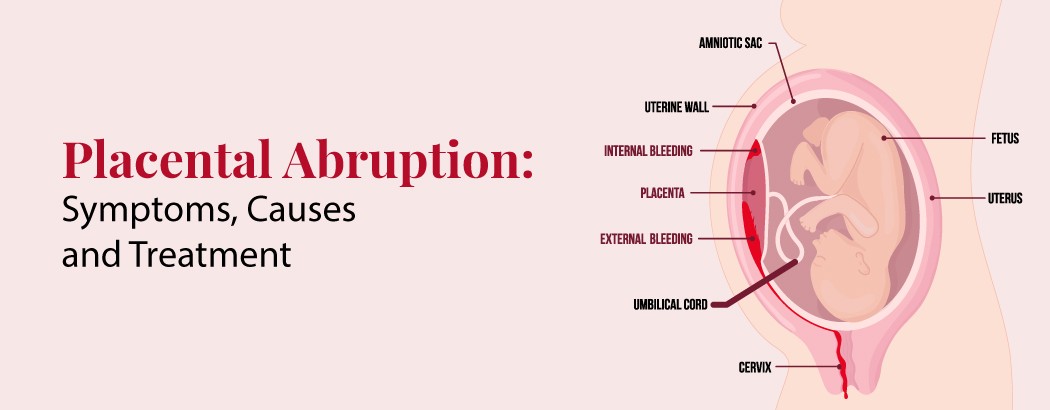
High blood sugar in women with gestational diabetes can affect them and their baby. For the mother, it increases the risk of premature delivery and preeclampsia, or pregnancy-induced high blood pressure.
High blood sugar in the mother can cause the baby to grow too large. Very large babies may get stuck in the birth canal and have birth injuries. Large size also increases the chances of needing a cesarean (surgical) delivery.
High blood sugars in the mother may be a cause of stillbirth. Uncontrolled gestational diabetes also increases the risk of jaundice and breathing problems in the newborn.
After birth, the baby may develop low blood sugar (hypoglycemia), a potentially dangerous condition. While in the womb, the baby’s pancreas produces large amounts of insulin in response to the mother’s high blood sugar, and it continues to do so after delivery. Without the sugar supplied by the mother, the excess insulin can cause the baby’s own glucose level to drop too low.
Possible symptoms of gestational diabetes
- Increased thirst and urination
- Fatigue (feeling tired all the time)
- Blurred vision
- Infections of the bladder, vagina, or skin
How is gestational diabetes treated?
Eating a healthy, well-balanced diet, maintaing a healthy weight, and getting regular exercise are important in preventing and treating gestational diabetes. Your health care provider will carefully monitor your blood sugar and may also refer you to an expert, such as an endocrinologist or diabetes educator, to help you keep your blood sugar under control. If diet and exercise are not enough, you may need treatment with oral medications or insulin.
Because women who have had gestational diabetes are at risk for developing type 2 diabetes, you should check your blood glucose six weeks after your baby is born and have regular check-ups after that. Breastfeeding can also reduce your child’s chances of becoming overweight and developing type 2 diabetes themselves.
Questions to ask your doctor
- What can I do to prevent gestational diabetes?
- I have gestational diabetes. How often should I check my blood glucose level?
- How often should I check my blood glucose after my baby is born?
- Can gestational diabetes lead to other health problems?
- Should I see an endocrinologist for my care?